Introduction
Background
The federal Medicaid program provides matching funds to states to pay for the medical treatment of low‑income individuals. The State participates in the federal Medicaid program through its California Medical Assistance Program, known as Medi‑Cal, which provides health care services to aged, disabled, and low‑income beneficiaries. The California Department of Health Care Services (Health Care Services) is the single state agency responsible for administering Medi‑Cal.
Medical providers participating in Medi‑Cal receive payments under this program through one of two delivery systems: fee‑for‑service and managed care. Under the fee‑for‑service system, providers render services to Medi‑Cal beneficiaries and then submit claims for payment. Under the managed care system—which is organized to manage the cost, utilization, and quality of care—medical care is provided to beneficiaries through Medi‑Cal managed care health plans (health plans). Specifically, Health Care Services pays health plans a fixed amount per month for each of their enrolled Medi‑Cal beneficiaries regardless of the quantity or types of medical services that the health plans deliver. The health plans, in turn, contract with medical providers. Plans are required to ensure that each enrolled beneficiary is assigned to a primary care physician who provides initial and primary care and whomay refer the enrollee to a specialist based on medical needs.
Although the State contracted with managed care plans as early as 1972, the federal Centers for Medicare and Medicaid Services (CMS) did not approve the first of the currently operating managed care programs—the County Organized Health Systems (COHS)—until 1983. In August 2005 CMS provided California with authority for a demonstration project that, among its other provisions, expanded health care coverage to the uninsured in certain California counties. This demonstration project was renewed in November 2010 and renamed the California Bridge to Reform, which includes most of the State’s existing Medi‑Cal managed care programs.
The number of Medi‑Cal beneficiaries increased considerably in 2014. Specifically, Health Care Services estimates that the changes the State made to Medi‑Cal eligibility requirements in response to the Patient Protection andAffordable Care Act (Affordable Care Act) resulted in more than 1.1 million additional Californians enrolling in Medi‑Cal through September 2014. In May 2014 the California Simulation of Insurance Markets—a joint project of th University of California, Berkeley, Center for Labor Research and Education and the University of California, Los Angeles, Center for Health Policy Research—estimated that by 2019 between 1.2 million and 1.3 million individualswill have signed up for Medi‑Cal because of the expansion enabled by the Affordable Care Act. Therefore, as Figure 1 below shows, it appears that most of the individuals projected to enroll in Medi‑Cal because of the program’s expansion have already done so.
Figure 1
Actual and Projected Additional Beneficiaries Enrolled in the California Medical Assistance Program Because of the Patient Protection and Affordable Care Act
From Implementation in 2014 Through 2019
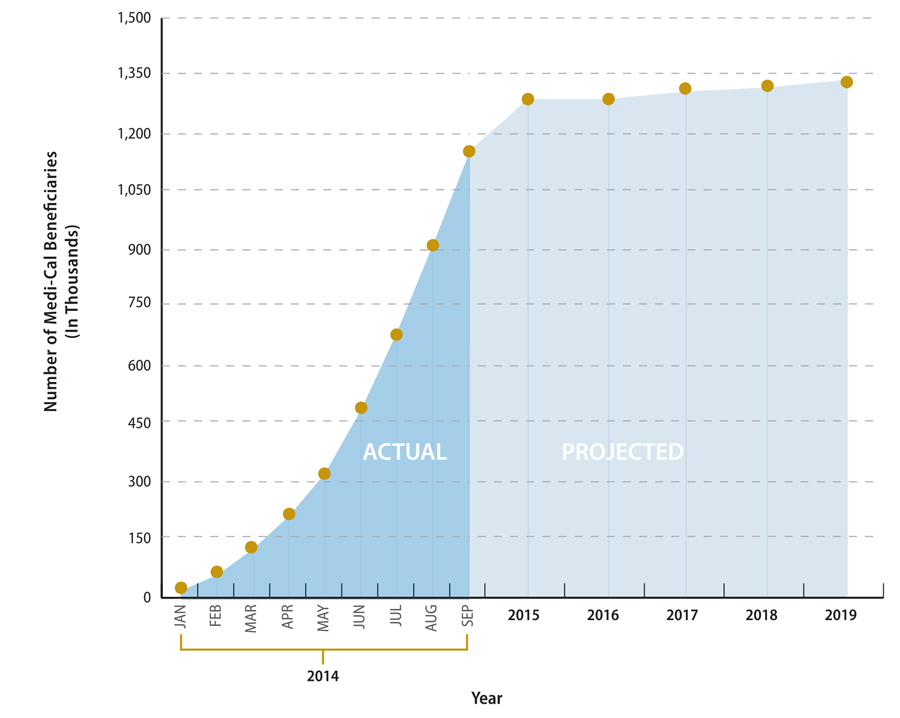
Sources: California Department of Health Care Services and the California Simulation of Insurance Markets, a joint project of the University of California, Berkeley, Center for Labor Research and Education and the University of California, Los Angeles, Center for Health Policy Research.
According to Health Care Services’ website, as of March 2015, more than 12.2 million Californians were enrolled in Medi‑Cal. About 9.2 million enrollees, or 76 percent of all Medi‑Cal enrollees, were in Medi‑Cal health plans. Health Care Services stated that the county in which a new enrollee resides determines whether the individual must enroll in managed care or whether he or she may choose to enroll in either a managed care or a fee‑for‑service health plan. When an individual applies for Medi‑Cal benefits, the county assigns an aid code that dictates the types of benefits to which the individual is entitled. Health Care Services further stated that a beneficiary required to enroll in Medi‑Cal managed care may be granted an exemption to remain temporarily in fee‑for‑service Medi‑Cal if warranted by the patient’s treatment plan, current medical status, or both. New beneficiaries in one county—San Benito County—may choose to enroll in either a managed care plan or fee‑for‑service Medi‑Cal. As we discuss here, only those counties that are part of the COHS model can offer a single plan to Medi‑Cal enrollees. The Social Security Act requires that beneficiaries have a choice of plans; CMS waived this requirement for the COHS model counties. Because San Benito County is not part of the COHS model and has only one health plan, the county offers fee‑for‑service to fulfill the federal requirement for choice.
Health Plan Options Available to Medi‑Cal Beneficiaries
California Medical Assistance Program (Medi-Cal)Managed Care Models Available to Counties
County‑Organized Health Systems: The California Department of Health Care Services (Health Care Services) contracts with a health plan created by the county board of supervisors.
Regional: Health Care Services contracts with two commercial plans.
Two-Plan: Health Care Services contracts with a county‑organized plan and a commercial plan.
Geographic Managed Care: Health Care Services contracts with several commercial plans.
Imperial: Health Care Services contracts with two commercial plans.
San Benito: Health Care Services contracts with one commercial plan.
Source: Health Care Services’ Medi-Cal Managed Care Program Fact Sheet.
The health plan options available to a Medi‑Cal beneficiary depend on the county in which the beneficiary resides. Counties ready for Medi‑Cal managed care worked with Health Care Services to determine the specific model of Medi‑Cal managed care that the county would follow. Each county participates in one of the six Medi‑Cal managed care models shown in the text box. The Medi‑Cal managed care model dictates the number and types of health plans offered to Medi‑Cal beneficiaries in a county.
For example, a county participating in the COHS model offers only one health plan, which is created by that county’s board of supervisors. Some COHS counties may choose to create their own locally initiated health plan; however, other counties may decide to join in a locally initiated plan. On the other hand, a county participating in the two‑plan model offers Medi‑Cal beneficiaries the option to choose from two plans—a locally initiated plan that is not part of the COHS model and a commercial plan licensed under the Knox‑Keene Health Care Service Plan Act of 1975 (Knox‑Keene Act). Figure 2 below shows the Medi‑Cal managed care model in which each county participates. Health Care Services stated that although it contracts with two commercial plans for both regional and Imperial models, Imperial County is not part of the regional model because the counties in the regionalmodel must be contiguous. One of the two health plans with which Health Care Services has contracted to serve beneficiaries in both the regional and Imperial models is the same, but the second plan in each model is different.
Figure 2
County Models for California Medical Assistance Program Managed Care

Source: California Department of Health Care Services’ website.
According to a chief in Health Care Services’ Managed Care Systems and Support Branch, once a county was ready for Medi‑Cal managed care, the county and Health Care Services entered into discussions to determine the best model for the county. Health Care Services then made a recommendation to CMS and the California Legislature to designate a particular model for the county. After approval from CMS and action by the Legislature, Health Care Services solicited bids, if applicable, and entered into contracts with health plans. Currently, Health Care Services contracts with seven commercial health plans, six plans created by counties participating in the COHS model, and nine locally initiated plans created by counties using the two‑plan model. Many of these 22 health plans operate in more than one county.4 Table 1 below shows the different health plans with which Health Care Services contracts toprovide services to Medi‑Cal beneficiaries in the State’s 58 counties.
| Type of medi‑cal managed health plan (Health Plan) | Health Plan | Number of Counties Served | Number of Enrollees |
|---|---|---|---|
| County‑Organized Health Systems | CalOptima | 1 | 741,076 |
| CenCal Health | 2 | 159,132 | |
| Central California Alliance for Health | 3 | 323,962 | |
| Gold Coast Health Plan | 1 | 186,744 | |
| Health Plan of San Mateo | 1 | 103,434 | |
| Partnership HealthPlan of California | 14 | 535,747 | |
| Local Initiative | Alameda Alliance for Health | 1 | 234,036 |
| CalViva Health | 3 | 307,613 | |
| Contra Costa Health Services | 1 | 154,970 | |
| Health Plan of San Joaquin | 2 | 294,707 | |
| Inland Empire Health Plan | 2 | 1,028,030 | |
| Kern Family Health Care | 1 | 194,767 | |
| L.A. Care Health Plan | 1 | 1,636,977 | |
| San Francisco Health Plan | 1 | 119,881 | |
| Santa Clara Family Health Plan | 1 | 221,522 | |
| Commercial | Anthem Blue Cross Partnership Plan | 28 | 686,436 |
| California Health and Wellness | 19 | 170,388 | |
| Care 1st Health Plan | 1 | 67,275 | |
| Community Health Group | 1 | 238,801 | |
| Health Net | 7 | 1,318,838 | |
| Kaiser Permanente | 5 | 115,706 | |
| Molina Healthcare | 5 | 405,392 | |
| Total | |||
Sources: The websites for the California Department of Health Care Services and Medi-Cal health plans.
The Monitoring Responsibilities of Health Care Services and the California Department of Managed Health Care
Health Care Services and the California Department of Managed Health Care (Managed Health Care) are responsible for assessing each health plan’s ability to serve enrollees. Federal regulations require Health Care Services to certify a health plan’s participation in the Medi‑Cal managed care program both at the initial entry and when new beneficiary populations are added to the program. Specifically, federal regulations require each health plan to demonstrate to the State that the health plan, among its other actions, maintains a network of providers that is sufficient in number, mix, and geographic distribution to meet the needs of the anticipated number of Medi‑Cal enrollees. Federal regulations also require the State to determine whether a network of providers is sufficient based partly on the numbers of providers and enrollees and on the time and distance for an enrollee to drive to a provider. Specifically, state law and regulations require a health plan to have at least one primary care physician in a health plan’s network (provider network) for every 2,000 Medi‑Cal enrollees. Further, Health Care Services’ contracts with health plans generally require health plans to have in their provider networks a primary care physician within 10 miles or 30 minutes of travel time from an enrollee’s place of residence.
Moreover, in accordance with the state Knox‑Keene Act, all commercial health plans and locally initiated health plans must obtain a license from Managed Health Care. In passing the Knox‑Keene Act, the Legislature intended topromote the delivery of quality health and medical care for Californians who enroll in a managed care health plan. Although the COHS plans do not require a license from Managed Health Care to serve Medi‑Cal beneficiaries, one plan has chosen to obtain a license for its Medi‑Cal product; therefore, the plan is subject to the provisions of the Knox‑Keene Act. To obtain a license from Managed Health Care, a health plan must file an application that includes enrollment projections, geographic area served, standards of accessibility, marketing, advertising, and current and projected financial viability. According to a health program specialist, Managed Health Care staff review the license application, recommend changes, and then allow the applicant to update its application. These reviews, changes, and updates continue until Managed Health Care’s review concludes that the applicant has met thelicensure requirements of the Knox‑Keene Act and Managed Health Care’s regulations.
The Knox‑Keene Act also requires Managed Health Care to perform reviews of all health plans it licenses at least once every three years. These reviews, generally referred to as routine surveys, must include reviews of the health plans’ procedures for obtaining health services, the procedures for regulating utilization, peer review mechanisms, internal procedures for assuring quality of care, and overall performance in providing health care benefits and meeting the health needs of the enrollees. At the discretion of its director, Managed Health Care also performs nonroutine surveys to protect the interests of managed care members. Managed Health Care initiates nonroutine surveys, which typically have specific and limited scopes, based on issues or concerns brought to its attention through various means, such as complaints from consumers.
Similarly, state law requires Health Care Services to perform annual medical audits of health plans using standards and criteria established under the Knox‑Keene Act. The purpose of these audits is to determine whether a health plan has the capacity, organization, and structure to fulfill its contractual obligations. As part of these audits, Health Care Services reviews essentially the same areas as those Managed Health Care reviews during its triennial routine surveys; however, unlike Managed Health Care, Health Care Services reviews the administrative and organizational capacity of the plan, and it does not review the plan’s language assistance program. We discuss the similarities in these reviews further here in the Audit Results.
Both Managed Health Care and Health Care Services maintain systems to address Medi‑Cal beneficiaries’ complaints related to health plans. State law requires Managed Health Care to maintain a toll‑free telephone number for the purpose of receiving complaints regarding health plans that it licenses. Generally, before filing a complaint with Managed Health Care, the enrollee must work with the health plan to resolve the issues. If the enrollee is not satisfied with the decision by the health plan or if the problem is urgent, the enrollee may file a written complaint with Managed Health Care. State law requires Managed Health Care to notify the complainant in writing of the resolution of the complaint within 30 calendar days. Moreover, state regulations allow Health Care Services to designate a Medi‑Cal Managed Care Office of the Ombudsman, which must investigate and resolve complaints received from Medi‑Cal beneficiaries about health plans.
Health Plan Provider Directories
State regulations require each individual enrolled in a Medi‑Cal health plan to select or be assigned a primary care physician. A primary care physician is a physician who has limited his or her practice of medicine to general health care or who is an internist, pediatrician, obstetrician‑gynecologist, or family practitioner. If the enrollee does not select a primary care physician within 30 days of enrollment, the plan must assign a primary care physician to him or her. Any enrollee dissatisfied with a primary care physician may select or be assigned to another primary care physician.
To aid each enrollee in making an informed decision when selecting a primary care physician and services covered by the enrollee’s health plan, Health Care Services’ contracts with health plans require that each health plan provide the individual with an enrollment package, including a directory listing all primary care physicians in the health plan’s provider network for the county in which the enrollee resides. Generally, the health plans also maintain searchable, online versions of their provider directories. Health Care Services’ contracts with health plans require that the provider directories include the name, address, and telephone number of each service location; the hours and days when each facility is open; the services and benefits available; and identification of providers that are not accepting new patients. Health Care Services requires the health plans to submit updated printed provider directories every six months for its review and approval to ensure that the directories contain appropriate, accurate, and complete information about primary care providers and other services available to plan members. Twice a year Health Care Services selects a sample of providers from a health plan’s directory and contacts them to verify whether the information about the providers included in the directory is accurate.
Scope and Methodology
The Joint Legislative Audit Committee directed the California State Auditor to perform an audit of the State’s Medi‑Cal managed care program to determine whether Health Care Services and Managed Health Care have an appropriate framework of oversight, guidance, and assistance in place to ensure that Medi‑Cal health plans have accurate provider directories and an adequate provider network to serve Medi‑Cal beneficiaries.
| AUDIT OBJECTIVE | METHOD | |
|---|---|---|
| 1. | Review and evaluate the laws, rules, and regulations significant to the audit objectives. | Reviewed relevant state and federal laws and regulations significant to the audit objectives. |
| 2. | For both the California Department Health Care Services (Health Care Services) and the California Department of Managed Health Care (Managed Health Care), determine whether these departments have an appropriate regulatory framework of oversight, guidance, and assistance in place to ensure that the California Medical Assistance Program (Medi‑Cal) managed care health plans (health plans) have accurate provider directories and an adequate network of providers to serve Medi-Cal beneficiaries. Specifically: | |
|
a. Determine how these departments provide oversight and ensure that health plans have accurate provider directories and adequate provider networks. |
To determine how Health Care Services and Managed Health Care provide oversight and ensure that health plans have accurate provider directories, we did the following:
To determine how Health Care Services and Managed Health Care provide oversight and ensure that health plans have adequate provider networks, we did the following:
|
|
|
b. Evaluate whether these departments have sufficient staff and resources and appropriate evaluation tools to monitor and ensure that health plans keep provider directories up to date and maintain adequate provider networks. |
To determine whether these departments have sufficient staff and resources, we did the following:
To determine whether these departments have appropriate evaluation tools to monitor and ensure that health plans keep up-to-date provider directory and adequate provider networks, we reviewed network adequacy evaluation tools and a provider directory review tool to determine if they were effective. |
|
| c. Identify and evaluate the sufficiency of these departments’ programs, policies, and procedures for ensuring health plans have accurate provider directories. |
Managed Health Care does not regularly perform procedures to ensure the accuracy of provider directories. |
|
| d. Determine the circumstances under which these departments would require health plans to provide verification of submitted provider network data. | Interviewed managers at Health Care Services and Managed Health Care and reviewed relevant documentation to determine the extent to which the two departments require verification of submitted provider network data. | |
| 3. | Determine whether Health Care Services and Managed Health Care have policies and programs in place to ensure that health plans are adequately meeting the health care needs of Medi-Cal beneficiaries. | Based on the steps described for Audit Objective 2, we assessed the adequacy of Health Care Services’ and Managed Health Care’s policies and programs to ensure that health plans are meeting the health care needs of Medi-Cal beneficiaries. |
| 4. | Select three health plans from three different counties to determine how they ensure adequate access to medical providers for the populations they serve. Specifically, determine the following: |
Selected health plans to capture different types of plans participating in the program across the State. We focused on the counties with a relatively larger beneficiary population within each selected health plan. We selected Health Net in Los Angeles County, Anthem Blue Cross in Fresno County, and Partnership HealthPlan of California in Solano County. For these health plans, we did the following to address the specified items: |
| a. Whether provider directories that the health plans submit to Health Care Services and Managed Health Care are accurate and comply with federal and state laws and regulations. |
|
|
| b. Whether provider directories the health plans provide to consumers and enrollees are consistent with Health Care Services’ internal records of providers that serve Medi-Cal health beneficiaries. |
Nothing significant came to our attention. |
|
| c. Assess, to the extent possible, whether the health plans perform ongoing oversight to ensure Medi‑Cal beneficiaries have adequate access to providers. |
Nothing came to our attention to suggest that these processes were not adequate. |
|
| d. Determine, to the extent possible, how often the health plans review the accuracy of their provider lists and ensure that each provider listed participates in Medi-Cal and is accepting Medi-Cal patients. |
|
|
| e. Evaluate, to the extent possible, the health plans’ practices to assist Medi-Cal beneficiaries who have trouble locating a provider. |
We found that the three health plans adequately addressed the beneficiaries’ requests for assistance. |
|
| f. Evaluate, to the extent possible, the process the health plans use to recruit and retain providers. |
We present these processes in Appendix B. |
|
| 5. | Review and assess any other issues that are significant to the accuracy of provider directories and the adequacy of the networks of providers for individuals enrolled in the Medi-Cal health plan. | To determine whether Health Care Services and Managed Health Care addressed complaints from Medi-Cal beneficiaries in a timely and appropriate manner, we performed the following:
|
Sources: California State Auditor’s analysis of the Joint Legislative Audit Committee’s audit request number 2014‑134 and information and documentation identified in the column titled Method.
Assessment of Data Reliability
In performing this audit, we obtained electronic data files extracted from the information systems listed in Table 3. The U.S. Government Accountability Office, whose standards we are statutorily required to follow, requiresus to assess the sufficiency and appropriateness of computer‑processed information that we use to support our findings, conclusions, or recommendations. Table 3 describes the analyses we conducted using data from these information systems, our methodology for testing them, and the conclusions we reached as to the reliability of the data. Although these determinations may affect the precision of the numbers we present, there is sufficient evidence in total to support our audit findings, conclusions, and recommendations.
| Information System | Purpose | Method and Result | Conclusion |
|---|---|---|---|
California Department of Managed Health Care (Managed Health Care) Clarify Managed Health Care’s Medi-Cal grievance data for 2013 and 2014 |
To select five grievances for testing the timeliness and appropriateness of their resolutions. |
|
Complete for the purpose of this audit. |
|
California Department of Health Care Services’ (Health Care Services) Medi-Cal Managed Care Office of the Ombudsman (ombudsman office) AT&T Call Management Call management data containing the Ombudsman office’s contact and case statistics for January 2013 through January 2015 |
To identify trends in ombudsman office contacts and cases from January 2013 through January 2015. | We did not perform accuracy and completeness testing on these data because testing the number and variety of data systems used in this audit would be cost‑prohibitive. | Undetermined reliability for the purposes of this audit. Although these determinations may affect the precision of the numbers we present, there is sufficient evidence in total to support our audit findings, conclusions, and recommendations |
Sources: California State Auditor’s analysis of various documents, interviews, and data obtained from Managed Health Care and Health Care Services.
Footnotes
4 Health Care Services has also contracted with two additional health plans to provide specialized services, such as AIDS care, to fewer than 1,000 Medi‑Cal patients. Our audit did not include these two plans and instead focused on health plans providing nonspecialized services. Go back to text
Back to top