Audit Results
The California Department of Health Care Services Did Not Verify Important Provider Network Data for the California Medical Assistance Program Managed Care Health Plans
The California Department of Health Care Services (Health Care Services) should improve its processes for verifying the data that it uses to assess whether the networks of primary care physicians (provider networks) establishedby the California Medical Assistance Program (Medi‑Cal) managed care health plans (health plans) are adequate. Federal regulations require, among other things, that the State certify a health plan’s participation in the Medi‑Cal managed care program. Before it issues this certification, Health Care Services requires the health plan to provide an analysis demonstrating that its provider network meets certain standards for the accessibility of its services to the health plan’s enrollees. Health Care Services has processes to verify some information, such as confirming a sample of contracted providers and recalculating certain ratios based on some of its own data. However, Health Care Services’ certification process does not include verifying the data used to demonstrate the adequacy of a health plan’s provider network. Further, for each health plan already certified to participate in Medi‑Cal managed care, Health Care Services also performs quarterly reviews of provider network adequacy through agreements with the California Department of Managed Health Care (Managed Health Care). As with its certification process, however, Health Care Services does not verify the accuracy of the provider network data it receives from the health plans and provides to Managed Health Care for the quarterly reviews. Without first verifying the provider network data, Health Care Services cannot be certain that the health plans maintain adequate provider networks to meet the medical needs of Medi‑Cal beneficiaries enrolled in those health plans.
Health Care Services Has Certified Health Plans’ Provider Networks Without Verifying the Underlying Provider Network Data
Federal regulations and Health Care Services’ contracts with health plans outline standards for provider network adequacy that health plans must follow to participate in the Medi‑Cal managed care program. Federal regulationsrequire, among other things, that the State certify a health plan’s participation in the program both at the health plan’s entry and when new beneficiary populations are added to the program. Additionally, federal regulations mandate that each health plan provide the State with documentation demonstrating that the health plan’s services are available and accessible to the expected number of beneficiaries in the health plan’s service area. Health Care Services has defined this accessibility in its contracts with health plans. The contract terms, in part, require health plans to maintain a network of primary care physicians so that at least one provider is located withineither 30 minutes or 10 miles of each enrollee’s residence unless Health Care Services has approved an alternative time‑and‑distance standard. Health Care Services most recently certified health plans when the State eliminated the Healthy Families Program and moved most of its participants into health plans within Medi‑Cal.5
For this recent certification, Health Care Services obtained approval from the federal Centers for Medicaid and Medicare Services (CMS) to move the beneficiaries of the Healthy Families Program into Medi‑Cal beginning in January 2013. In its approval of the transition, CMS required the State to demonstrate certain activities, such as the health plans’ successful provision of coverage to children and their provider network adequacy. For example,CMS required that before implementing the transition, the State had to estimate the percentage of Healthy Families Program beneficiaries it anticipated would be able to keep their current primary care providers after the transition. We reviewed three health plans—Anthem Blue Cross in Fresno County, Health Net in Los Angeles County, and Partnership HealthPlan of California (Partnership HealthPlan) in Solano County—during this audit. For the three health plans we reviewed, Health Care Services stated in its certification to CMS that each of the plans had a sufficient provider network in place to provide all primary care physicians necessary to transitioning HealthyFamilies Program enrollees. Health Care Services also stated that these health plans could provide a high number of enrollees transitioning from the Healthy Families Program with the ability to maintain their current health care providers. However, Health Care Services did not verify some of the data that informed these certifications.
In February and April 2013, Health Care Services certified to CMS that the three health plans we reviewed would have available services; it based this certification on the number of providers in the health plans’ provider networks who participated both in the Healthy Families Program and in existing Medi‑Cal health plans. Health Care Services analyzed the provider network data it obtained from the three health plans we reviewed to determine which providers in their Healthy Families Program networks overlapped with providers in their Medi‑Cal networks. However, Health Care Services did not verify that the provider network data it received from the health plans wereaccurate. Instead, it relied on the health plans’ electronic certification that the data submitted were accurate. Nevertheless, reliance on this type of certification is not a sufficient substitute for performing some verification of accuracy. Health Care Services also supplied a report on the Healthy Families Program transition to Medi‑Cal that offered detailed statistics about the ability of these three health plans to participate in this transition, such as the percentage of primary care physicians who were not accepting new patients and the percentage of Healthy Families Program beneficiaries who could keep their primary care providers. However, Health Care Services could not show documentation indicating how it calculated these values from the health plans’ data. As a result, Health Care Services cannot support with accurate data that it ensured that these health plans had adequate provider networks for the transition of Healthy Families Program beneficiaries to Medi‑Cal health plans.
In addition to using health plan data, Health Care Services also based its certifications on other factors, including qualitative factors. For example, Health Care Services provided CMS with the survey responses from the three health plans that identified how the plans would ensure the continued care of beneficiaries who could not maintain their primary care providers. The survey also asked health plans to provide a description of their effortsto contract with the Healthy Families Program providers who were not already in the health plans’ Medi‑Cal provider networks. Health Care Services also met the federal requirements for provider network adequacy related to including specific terms in its contracts with the three health plans we reviewed, such as requiring the plans to offer services to enrollees 24 hours a day, seven days a week when medically necessary. Further, CMS required theState to ensure that each plan has an accessible network with reasonable geographic proximity to beneficiaries. Health Care Services indicated in its certification that because there was no geographical expansion of coverage, only a population expansion, it performed limited review in this area—comparing the Healthy Families Program’s provider network with the health plans’ provider networks to ensure there would be the same coverage.
We also selected and reviewed one initial plan certification completed in 2013 for California Health and Wellness—a health plan that now serves Medi‑Cal managed care beneficiaries in Imperial County. When the State expanded Medi‑Cal managed care into 28 rural counties in 2013, federal regulations required the State to determine, among other things, whether the health plans that wanted to participate in Medi‑Cal managed care in these counties had the numbers of providers required to furnish services to beneficiaries as well as a provider network at locations within the time‑and‑distance standards. State law covering health plans that are licensed under the Knox‑Keene Health Care Service Plan Act of 1975 (Knox‑Keene Act) requires health plans to have at least one primary care physician for every 2,000 beneficiaries. Moreover, Health Care Services’ contracts with health plans require them to maintain a provider network of primary care physicians located within 30 minutes or 10 miles of members’ residences unless the health plan has an alternate time‑and‑distance standard approved by Health Care Services.
In certifying California Health and Wellness, Health Care Services reviewed various areas related to provider network adequacy. For example, it verified that the health plan had enough primary care physicians to accommodate the expected number of plan beneficiaries. Health Care Services also used the number of beneficiaries in Imperial County to calculate the minimum number of primary care physicians needed to maintain a ratio of at least one provider for every 2,000 beneficiaries. Further, it verified plan data on the number of primary care physicians by obtaining written agreements between primary care providers and California Health and Wellness. Health Care Services reported that it reviewed 5 percent of all primary care physicians, or nine providers, claimed by the health plan. Health Care Services also reviewed the expected utilization of services for the health plan and whetherproviders were accepting new patients.
However, Health Care Services did not verify the data that California Health and Wellness used to demonstrate that it met the time‑and‑distance standards. Health Care Services required the health plan to submit a geographic access report to demonstrate that it met the time‑and‑distance standards. This report included a map showing the parts of the health plan’s service area that its provider network could serve, taking into account the required time‑and‑distance standards. The report also included a summary of the number of enrollees in the service area who would not have access to the health plan’s provider network within the required time‑and‑distance standards. This geographic access report’s information allowed Health Care Services to determine whether the health plan needed to take any steps to mitigate the lack of accessibility, such as providing transportation services to enrollees. Because some providers practice at multiple locations, this report took into consideration the multiple locations where the health plan’s providers practiced. However, Health Care Services’ review tool for geographicaccess reports does not include a step directing staff to verify the number of provider locations that the health plan used in its geographic access report. It is important for Health Care Services to verify the providers’ location information so that it can ensure that health plans provide enrollees with adequate access to providers.
The acting chief of Health Care Services’ Managed Care Operations Division (acting chief) believes its existing processes for certifying initial provider networks are adequate and does not believe that health plans are misstating their provider networks in the geographic access reports. Further, Managed Care Systems and Support Branch staff cited an analysis that Health Care Services performs on zip codes that do not have appropriate coverageby primary care providers. However, Health Care Services performs this analysis only when a health plan identifies gaps in provider coverage based on the health plan’s geographic access report. Managed Care Systems and Support Branch staff further cited another review that Health Care Services performed comparing the provider network it approved under Medi‑Cal’s fee‑for‑service plans and the network certification that we reviewed. Health CareServices’ review found that the provider network that the plan proposed had 109 providers in common with the fee‑for‑service provider network. However, because the health plans included providers who might not have participatedin Medi‑Cal’s fee‑for‑service plans, Health Care Services’ comparison of the two provider networks would not have ensured the accuracy of the health plans’ provider network data.
Health Care Services Does Not Verify the Accuracy of the Data Used for the Required Ongoing Assessments of Provider Networks
In addition to performing initial reviews of provider network adequacy, Health Care Services has established agreements with Managed Health Care, as state law requires, to perform ongoing reviews of provider network adequacy. The agreements require Managed Health Care to assess quarterly the adequacy of provider networks, and these assessments are to include a review of current geographic access for plan members using data that Health CareServices obtains from the health plans and forwards to Managed Health Care. Upon completing its assessment, Managed Health Care is required under the agreements to provide the results to Health Care Services.
However, Health Care Services does not verify the accuracy of the provider network data it receives from health plans and sends to Managed Health Care. Specifically, Health Care Services issued a policy letter in March 2014 requiring each existing health plan to submit monthly its provider file, which includes the health plan’s provider network data, such as the names and addresses of providers. The policy letter also specifies the methods the health plans should use to organize and submit their monthly file of provider data, and it states that the data submission requirement will help Health Care Services ensure the accuracy of the provider data and the adequacy of health plans’ provider networks. Because Health Care Services is obligated by its agreement to provide these data to Managed Health Care to use in determining whether a health plan continues to have an adequate provider network, we would expect Health Care Services to review the data, at least on a sample basis, to verify their accuracy. For example, it could verify the address information of a sample of providers included in the health plan’sdata by contacting providers directly. However, Health Care Services does not review the data before it forwards the information to Managed Health Care even though such reviews would enable Health Care Services to have confidence in the data it receives from the health plans.
Without verifying the accuracy of the provider network data received from the health plans, Health Care Services cannot be certain that the health plans have adequate provider networks that meet the access standards that aimto help health plan beneficiaries find and receive healthcare. Whether initially certifying the health plan or providing data to Managed Health Care for the quarterly reviews, Health Care Services is vulnerable to inaccurate provider network analyses because it does not have processes for verifying this information. Ensuring that the health plans are not overstating their provider network data is especially important considering that our review of provider directories found that one health plan’s directory listed providers who no longer participate in that plan, as we discuss here. Health Care Services’ lack of a process to verify the accuracy of the data it uses to determine the adequacy of provider networks could lead to an incorrect conclusion about a health plan’s ability to provideMedi‑Cal beneficiaries with timely access to medical care.
Characteristics of Medi‑Cal Managed Care Health Plans’ Data About Providers That the California Department of Health Care Services Intends to Verify
- Accuracy—The California Department of Health Care Services (Health Care Services) intends to compare provider data entries to other provider data, such as plan financial records.
- Completeness—Health Care Services intends to compare provider data to external sources, such as providers’ contracts with the California Medical Assistance Program (Medi‑Cal) managed care health plans (health plans).
- Reasonableness—Health Care Services intends to compare a health plan’s entire data set against reasonable standards or expectations.
- Timeliness—Health Care Services intends to compare provider data entries to other available data, such as information on contract execution dates. For example, it intends to compare the contract execution date to the month that the health plan included the provider in its data submission.
Sources: Chief of Health Care Services’ Program Monitoring and Compliance Branch within the Medi‑Cal Managed Care Quality and Monitoring Division as well as its April 2015 Network Adequacy Monitoring Project outline
The chief of Health Care Services’ Program Monitoring and Compliance Branch (branch chief) stated that when Health Care Services receives the provider files from the plans, it ensures that the data fields are filled in, but it does not perform any further process or quality checkon the data. He acknowledged that Health Care Services has identified this omission as an area for improvement and stated that Health Care Services has included it as a component of its project plan to revamp its monitoring of provider network adequacy. Specifically, the project plan, scheduled for implementation in the latter part of 2015, includes Health Care Services’ establishing a processto verify the data in the provider files submitted by the health plans. Further, the branch chief noted that Health Care Services’ project plan requires the establishment of a process to validate submissions of provider data files and that its measuringthe quality of provider data files will likely act as an incentive for health plans to submit quality data. As the text box shows, Health Care Services plans to verify the accuracy, completeness, reasonableness, and timeliness of the provider data it receives from the health plans.
Health Care Services Has Not Ensured That Medi‑Cal Managed Care Health Plans Publish Accurate Provider Directories
The three health plans we reviewed included inaccurate information in their provider directories, and Health Care Services’ review did not identify these inaccuracies before it approved the directories’ publication. We foundmany errors in the directories, including errors related to providers’ telephone numbers and addresses as well as to whether the providers were accepting new patients. Although all three health plans indicated that they rely onproviders to notify them of changes, we found that the two health plans that actively reached out to providers in their provider network to update information generally had fewer inaccuracies than did the one health planthat only recently began reaching out actively to providers to update itsinformation. When errors occur in the providers’ directories, Medi‑Cal beneficiaries could experience delays in their access to care.
The Three Provider Directories We Reviewed Contained Varying Degrees of Inaccurate Information
Our review of provider directories for three health plans found that the directories did not always contain accurate data about providers, such as telephone numbers, addresses, or information about whether they were accepting new patients. We reviewed a statistically valid sample of providers for three Medi‑Cal managed care plans. Specifically, we reviewed certain information related to a sample of providers that Anthem Blue Cross includedin its provider directory for Fresno County and that Health Care Services approved in December 2014. We also reviewed information for a sample of providers included in Health Net’s provider directory for Los Angeles County andfor Partnership HealthPlan in Solano County that Health Care Services approved in August 2014. See Appendix A for further details on the process we used for this review, including the sample selection methodology and the questions we asked each provider we contacted.
Although the directories for all three health plans contained some inaccurate information, two of the three health plans’ directories contained errors related to several providers, while the third health plan, which lists fewer providers, contained only one error. Because the directories of the three health plans had varying numbers of providers, and because we used a statistically valid sample size, the number of providers we surveyed for each plan differed. Specifically, we found inaccuracies related to 18, or 23.4 percent, of the 77 providers we reviewed from Anthem Blue Cross’s provider directory for Fresno County. Similarly, for the 93 providers we sampled from Health Net’s provider directory, we found inaccuracies related to 11 providers, or 11.8 percent. In contrast, we found inaccuracies related to only one, or 3.1 percent, of the 32 providers we reviewed from Partnership HealthPlan’s provider directory.
Although we expected that a provider directory might contain some outdated information at anygiven time because of the time needed to update the information, our review identified many errors that did not seem reasonable because of the length of time that the errors were outstanding. For example, a telephone number for a provider listed in Anthem Blue Cross’s directory belonged to a personal residence, and the individual to whom we spoke informed us thatshe had been receiving calls from Anthem Blue Cross’s enrollees for more than a year. In another instance, a staff member for one of Anthem Blue Cross’s providers indicated that the provider’s office had moved two or three years ago, but the directory still reflected the old address. Further, staff at an office that was listed in Health Net’s directory told us that the provider had left the office in June 2014.
Based on the results of our testing, an estimated 3 percent to 23 percent of provider directory listings have inaccuracies in at least one of the six areas we reviewed. We consulted a statistician to verify our sample selection methodology and to help us project the errors in the provider directories. Table 4 provides a summary of the percentage of errors we found in ourtesting of six areas and our resulting projection of the number of provider directory listings that have incorrect information.
Each of the inaccuracy rates and projections we identify in Table 4 has a different margin of error. The margin of error is the uncertainty associated with an estimate that is based on datagathered from a sample of the population rather than from the full population. For example, we surveyed 93 of the 2,468 providers listed in Health Net’s provider directory for Los Angeles County. We were unable to reach two of the 93 providers because the telephone numbers listed for them in the provider directories were incorrect. We found that for six, or 6.6 percent, of the 91 providers’ offices we were able to reach, staff indicated that the listed provider was no longer practicing at that location or that they did not know the provider. Using this error rate, we project that the addresses for 163 of the 2,468 providers in this directory were incorrect. Although 6.6 percent represents our best estimate of the error rate for the entire directory, given a margin of error of plus or minus 5 percent, we estimate that the errors in the directory could represent as few as 39, or 1.6 percent, of provider listings or as manyas 286, or 11.6 percent, of provider listings.
| Number of Providers in Directory | Number of Providers Reviewed | Incorrect Provider Telephone Number | Incorrect Provider Name (Not At Address) | Incorrect Provider Address | Incorrect Practice Type (Pediatrics, Family Practice) | Provider Not Accepting Medi‑Cal Managed Care Health Plan (health plan) Coverage | Incorrect Provider Status (Open or Closed to New Patients) Providers With Incorrect | Information in One or More Areas Reviewed |
|---|---|---|---|---|---|---|---|---|
| Anthem Blue Cross—Fresno County* | ||||||||
| 383 | 77 | 5.2% | 6.8% | 5.9% | 3% | 4.5% | 7.5% | 23.4% |
| Projected number of provider directory listings with errors | 20 | 26 | 23 | 11 | 17 | 29 | 90 | |
| Health Net—Los Angeles County* | ||||||||
| 2,468 | 93 | 2.2% | 6.6% | 1.2% | 0% | 0% | 3.7% | 11.8% |
| Projected number of provider directory listings with errors | 53 | 163 | 30 | 0 | 0 | 90 | 292 | |
| Partnership HealthPlan of California—Solano County* | ||||||||
| 47 | 32 | 0% | 0% | 0% | 0% | 0% | 3.1% | 3.1% |
| Projected number of provider directory listings with errors | 0 | 0 | 0 | 0 | 0 | 1 | 1 | |
Source: California State Auditor’s analysis of testing results from its review of the accuracy of provider directories from three Medi-Cal health plans.
* The percentages represent our best estimates of the error rates in the provider directories, given a 95 percent confidence level. Each number has a unique margin of error.
During our review of the three health plans and their directories, we found that these health plans had updated their online provider directories to correct some of the inaccuracies we identified through our survey. We did not include these corrected inaccuracies in our error rates. For example, in reviewing the 77 providers listed in Anthem Blue Cross’s directory, we found inaccuracies related to six providers’ telephone numbers. However, when we consulted the health plan’s online directory, we found that the health plan had corrected the telephone number for one provider and removed another provider from its listings.
Health Plans’ Varied Processes for Reviewing Provider Directories Likely Account for the Differing Levels of Directory Errors
The process that each of the three health plans employs to update its provider directory may have contributed to the variations in the number of inaccuracies we found. The acting chief confirmed that Health Care Services does not specify the method that a health plan should use when verifying its provider network information. As a result, the three plans we reviewed verify this information in different ways even though each plan stated that it relies on providers to notify the health plan about any changes in their telephone numbers or physical addresses, whether the providers are accepting new patients, and other information. We found that each of the two health plans we reviewed that had a process for regularly reaching out to providers to update their information had fewer provider directory inaccuracies than the health plan that only recently began reaching out to providers.
Specifically, Partnership HealthPlan regularly contacts its providers to maintain updated directory information. According to its associate director of regulatory affairs, Partnership HealthPlan requires its providers to notify it within 30 days of any changes that affect the provider directory. In addition, Partnership HealthPlan’s procedures require its staff to visit each of its primary care providers eight to 10 times per year and to identify any changes in provider information during these visits. Using information gathered during these visits, the health plan actively updates its provider directory. The frequent interactions with its providers give Partnership HealthPlan a way to identify changes in provider information quickly, even if the provider fails to notify the health plan of the changes. In fact, as we discussed previously, of the 32 providers reviewed for SolanoCounty, we identified only a single error in the providers we reviewed. The Partnership HealthPlan associate director told us that it uses the same process for updating information related to 793 primary care physicians in its provider network for 14 counties serving Medi‑Cal beneficiaries.
Health Net’s process for updating provider information does not involve as many contacts with the providers as the process used by Partnership HealthPlan: Health Net’s provider network management director told us that HealthNet reaches out to each provider twice a year to verify or update provider information. She explained that Health Net staff perform multiple follow‑ups with providers, including faxing letters and contacting the provider’s medical group by telephone. She stated that Health Net aims to ensure that it obtains a response rate of at least 90 percent of providers, and it excludes providers from its directories who do not respond to this verification process. According to its Medicaid compliance manager, Health Net uses the same process for updating information related to the 3,575 primary care physicians in its provider network for all seven counties in which it serves Medi‑Cal beneficiaries.
However, the Medicaid compliance manager told us that Health Net staff did not fully follow the usual process of excluding nonresponsive providers when updating its Los Angeles County provider directory for August 2014, which was the directory we reviewed. She stated that the results of the directory update vary from previous results because Health Net received a poorer provider response to the multiple outreach initiatives than had occurred in the past. She noted that during that time Health Net had significant communication and outreach to the provider community related to other plan activities, including the Patient Protection and Affordable Care Act implementation and expansion of Medi‑Cal. These same activities led to an unusual increase in workload for its regional team and to deviation from the usual process. Health Net, therefore, included information about providers in its provider directory that it had not verified through its usual process. Specifically, according to its provider response spreadsheet, it did not receive a response rate of at least 90 percent from its Los Angeles County providers, and it did not exclude all nonresponsive providers from its August 2014 directory. As discussed previously, in our review of the accuracy of information in Health Net’s August 2014 provider directory for Los Angeles County, we identified errors in the information for 11 providers, or 11.8 percent of the 93 providers we reviewed. Health Net’s Medicaid compliance manager told us that it has taken steps to support consistent implementation ofits verification process, including holding meetings with the regional team to review the process; providing clarity on steps and responsibilities; increasing oversight, management, tracking, and monitoring; as well as process improvement activities.
Finally, the third health plan we reviewed—Anthem Blue Cross—only recently began actively reaching out to providers to update their information. Anthem Blue Cross’s director of business integration and contract administration (director) stated that beginning in the second quarter of 2014, it reached out to a large number of its commercial providers, who also often participate in Medi‑Cal, to update the health plan’s provider directoryinformation. However, we identified a large number of inaccuracies in Anthem Blue Cross’s October 2014 provider directory for Fresno County. Overall, we found one or more inaccuracies in provider information for 18, or 23.4 percent, of the 77 providers we reviewed. For example, three of the providers we reviewed reported to us that they had stopped accepting Anthem Blue Cross’s Medi‑Cal managed care insurance in July 2014. According to the director, the processes that the health plan uses to verify the accuracy of the provider directories are consistent across all counties. She stated that Anthem Blue Cross has 2,367 primary care physicians in its provider network for the 28 counties in which the health plan serves Medi‑Cal beneficiaries.
The director stated that Anthem Blue Cross began a new process in the second quarter of 2014 to reach out to a selection of its providers to confirm their provider directory information. She reported that Anthem Blue Cross reached out to almost 40,000 providers participating in its commercial provider network, many of whom often participate in Anthem Blue Cross’s provider network for Medi‑Cal. The director further stated that Anthem Blue Cross had implemented two additional processes during the fourth quarter of 2014. The first process involves mining data from different databases to capture provider demographic changes reported through claims, grievance, and appealsprocesses. In the second process, the plan reaches out to its contracted medical groups asking them to validate demographic information, provider rosters, and the groups’ ability to accept new Medi‑Cal managed care beneficiaries. The director stated that Anthem Blue Cross plans to perform these three new processes twice each year to coincide with Health Care Services’ requirement to update provider directories twice each year.
Health Care Services’ Process for Verifying the Accuracy of Provider Directories Is Inadequate
Although we found multiple errors in the provider directories for both Anthem Blue Cross and Health Net, Health Care Services—which stated that it reviewed the provider directories of the three health plans we examined—did not identify any inaccuracies. State law requires Health Care Services to ensure that certain health plans are able to maintain accurate information about a provider’s ability to accept new patients enrolled in Medi‑Cal managed care. Health Care Services’ policy requires plans to submit provider directories for its approval every six months, and one of the goals of the policy is to assure that provider directories contain appropriate, accurate, and complete information. Such information enables each enrollee to obtain a primary care provider without unnecessary delay.
Health Care Services has not ensured that staff follow a consistent methodology for selecting the number of providers to review and for verifying the accuracy of the health plans’ directories. Health Care Services’ directory review tool, which guides its review of the accuracy of provider directories that health plans submit for approval, is inadequate. Specifically, the tool guides staff who review the directories for the required format and content. However, the tool does not include guidance on selecting an appropriate sample of providers to review. A Medi‑Cal Managed Care section chief (section chief) at Health Care Services told us that staff generally review the lesser of 25 providers or 10 percent of all providers included in the directories that staff approve. However, the practice varies among the staff reviewing directories covering different health plans. For example, Health Care Services confirmed that staff reviewed 25 of the providers listed in Anthem Blue Cross’s Fresno County directory and 10 percent of providers in Partnership HealthPlan’s Solano County directory. In contrast, the contract manager responsible for conducting the review of Health Net’s August 2014 Medi‑Cal provider directory for Los Angeles County confirmed that she reviewed 5 percent of the providers listed, or well over 100 primary care providers.
Additionally, Health Care Services does not require staff to use a consistent methodology for sample selection to ensure that they review a sufficient variety of providers to determine whether the health plans’ directories are accurate. According to the section chief, some staff members pick one to three providers in a particular specialty—such as pediatrics—from each city listed in the directory under their review. The section chief noted that other staff pick a number, such as 12, and select every 12th provider listed in the directory. Still other staff members choose odd‑ or even‑numbered pages and randomly select variable numbers and types of providers listed on those pages. Because the goal of Health Care Services’ review of provider directories is to ensure accuracy and completeness of the entire directory, we expected Health Care Services to use a consistent, statistically valid random sample like the one we used in our survey of providers. When Health Care Services does not require its staff to use a statistically valid random sample, it has less assurance that it is identifying effectively the extentto which errors exist in the provider directories that it reviews.
Health Care Services also could not demonstrate that it performed reviews to verify the accuracy of the three provider directories we reviewed. Although Health Care Services claimed that it did not identify errors in these provider directories, when we asked Health Care Services for the documentation of its reviews, the section chief stated that his staff did not retain this documentation. For example, on December 23, 2014, in response to our request for documentation, the section chief informed us that his staff had reviewed Anthem Blue Cross’s October 2014 provider directory that same day. However, he stated that his staff did not keep any documentation of the review. The acting chief confirmed that Health Care Services maintains only the documentation associated with errors it identifies during its reviews of provider directories. Because Health Care Services did not identify any errors in the provider directories we reviewed, it did not maintain any documentation associated with its reviews. The acting chief further stated that the reason staff did not retain documentation associated with their reviewsis that there is no requirement to do so. However, we believe that it would be a good business practice for Health Care Services to require staff to document provider directory reviews and to guide them in the review process so that the department can demonstrate its oversight efforts.
Further, Health Care Services did not always maintain documentation for its approvals of those directories. Specifically, for two of the health plans we reviewed, Health Care Services could not provide documentation of its communications with the health plans regarding its provider directory approval. In these instances, we obtained the documentation of approval communications directly from the health plans. According to the acting chief, Health Care Services did not maintain these communications because it is not required to do so. Whether maintaining evidence of provider directory approvals is required or not, we believe that doing so would be a good business practice for Health Care Services.
When health plans’ provider directories contain inaccurate information, Medi‑Cal managed care beneficiaries may experience difficulties in obtaining timely access to care. For example, beneficiaries may not be able to contact providers, or beneficiaries may show up at the wrong locations, causing delays in their receiving medical care. Health plans may also assign beneficiaries to providers who are listed as accepting new patients when,in fact, the providers are closed to new patients. This situation may result in Medi‑Cal beneficiaries’ inability to get timely appointments with providers. Further, the fact that 4.5 percent of the Anthem Blue Cross providers whose directory listings we reviewed were no longer accepting Medi‑Cal insurance raises a question as to whether the size of Anthem Blue Cross’s provider network is overstated. Health Care Services agreed that it can enhance its processes to better identify and correct directory inaccuracies.
Health Care Services Cited a Lack of Resources for Its Inability to Respond to All Inquiries or Requests for Assistance From Medi‑Cal Beneficiaries
According to the chief of Health Care Services’ Medi‑Cal Managed Care Office of the Ombudsman (ombudsman chief), the office has lacked adequate resources to handle all the telephone calls it receives from Medi‑Cal beneficiaries. As Figure 3 below shows, between February 2014 and January 2015 the telephone system for the Medi‑Cal Managed Care Office of the Ombudsman (ombudsman office) gave busy signals to callers, rejecting from about 7,000 to more than 45,000 calls per month. During this period, an average of 12,500 additional calls also went unanswered each month because of staffing limitations. Moreover, the Managed Care Internal Operations Branch chief stated that when the telephone system and the staff were able to answer calls, the ombudsman office lacked an adequate database to track those calls.
Figure 3
Number of Contacts From January 2013 Through January 2015 That the California Department of Health Care Services Received
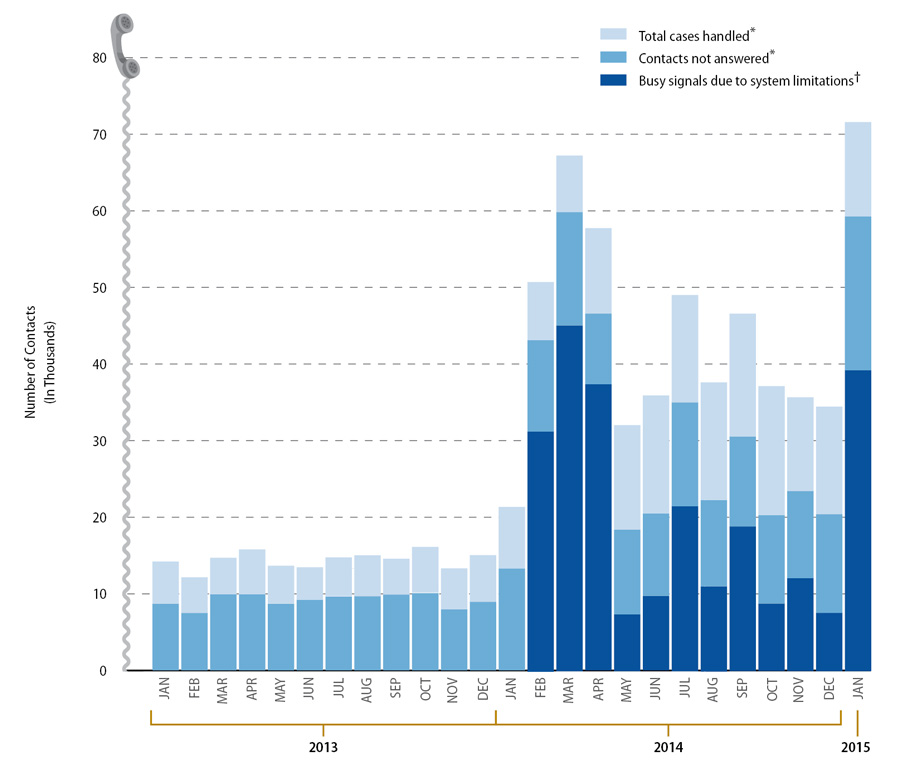
Source: Call center data from the California Department of Health Care Services’ (Health Care Services) California Medical Assistance Program Managed Care Office of the Ombudsman (ombudsman office).
Note: Please refer to the Introduction’s Scope and Methodology for our assessment of the reliability of data used to create this figure.
* In addition to telephone calls, contacts and cases after July 2014 include email contacts that the ombudsman office received. The ombudsman office estimates that 5 percent of contacts came from these emails.
† According to the phone service provider for Health Care Services, the phone service could not provide information on busy signals before February 2014.
State regulation allows Health Care Services to designate a Medi‑Cal managed care ombudsman who investigates and resolves complaints about managed care plans by or on behalf of Medi‑Cal beneficiaries. Some of the calls that the ombudsman office receives include calls from Medi‑Cal beneficiaries who have concerns related to their access to health care or complaints regarding the services provided by the health plan. However, according to the ombudsman office’s staff, the office’s telephone system cannot handle the volume of calls that the ombudsman office receives. Specifically, the ombudsman chief provided data showing that the ombudsman office receives anywhere from 32,000 to more than 71,000 calls for assistance each month. She stated that the telephone system can handle only 25,000 calls per month. As a result, many callers cannot get through the telephone system to speak with ombudsman office staff. The acting chief stated that Health Care Services is in the final phases of upgrading its telephone system for the ombudsman office, with full implementation expected by June 30, 2015. He stated that thenew telephone system will not limit the number of telephone calls that the ombudsman office can receive each month. Further, the new system will have an automated system to route the caller to the proper analyst by using a combination of factors, including the agent’s availability to accept calls and the agent’s skill level. He stated that the system will also have a queuing function that can prioritize calls based on their time in the queue.
Moreover, the ombudsman chief stated that the ombudsman office’s staffing limitations have led it to answer an average of only 30 percent to 50 percent of the calls that the telephone system has accepted. She stated that although calls that go unanswered within 18 minutes’ wait time are directed to a voicemail service, the ombudsman office lacks staffing capacity to answer these messages. The ombudsman chief noted that the office does not know whether the calls that the telephone system does not accept or that staff cannot answer correspond to new cases that never get addressed or are associated with multiple repeat calls by limited numbers of individuals for cases that the ombudsman office eventually handles and resolves. Figure 3 depicts the monthly discrepancies between the numbers of phone calls placed to the ombudsman office’s call center and the numbers of callsanswered from January 2013 through January 2015.
According to the chief of the Managed Care Internal Operations Branch, in addition to limitations of the telephone system and staff, the ombudsman office has lacked an adequate database to track all calls that its staff are able to answer. Specifically, he stated that the staff have maintained in a database the information related to all calls answered. Health Care Services’ management has reviewed these data periodically to identify trends specifically related to the resolution of the calls in order to train staff regarding current issues. However, the ombudsman chief stated that because of hardware limitations, the database has crashed frequently, resulting in loss of data related to the contacts the staff may be addressing at the time. She further indicated that the ombudsman office’s practice has been for the analyst to attempt to reenter the information that was lost during a system crash to minimize the amount of information that is lost. The chief of Managed Care Internal Operations Branch estimated that the database has lost information related to 10 to 20 calls each month. The ombudsman chief also stated that Health Care Services was in the process of upgrading the database to ensure data integrity, and the acting chief stated that Health Care Services upgraded its server software in March 2015 and plans to have an updated system in place during fiscal year 2015–16.
Health Care Services Needs to Improve Its Monitoring of Health Plans
Health Care Services has not monitored health plans adequately to ensure that they meet Medi‑Cal beneficiaries’ medical needs. Specifically, Health Care Services has not performed, as required by state law, annual medical audits of all Medi‑Cal health plans to evaluate the overall performance of the health plans in providing health care benefits to enrollees. Also, Health Care Services has not always ensured that Managed Health Care has performed all the required quarterly assessments that it contracted to provide. As a result, Health Care Services cannot verify adequately that health plans are ensuring that Medi‑Cal beneficiaries have adequate access to care.
Health Care Services Has Not Completed Annual Medical Audits of Health Plans as State Law Requires
Health Care Services has not complied with a statutory requirement to perform annual medical audits of Medi‑Cal health plans. Specifically, state law requires Health Care Services to perform annual medical audits of all Medi‑Cal health plans to evaluate the overall performance of the health plans in providing health care benefits to their enrollees. However, according to the chief of Health Care Services’ Medical Review Branch, Health Care Services did not perform any annual medical audits before 2012. He stated that he was advised of the legal requirementfor annual medical audits once he assumed the position of chief in May 2011, and he immediately began addressing the issue. Specifically, he stated that he began assembling audit staff capable of performing the annual medical audits, and this effort included redirecting approximately 40 percent of existing staff and training them.
As staff completed training, they were able to perform some of the annual medical audits. Nonetheless, Health Care Services has not yet fully complied with the statutory requirement for annual medical audits. Specifically, Health Care Services contracts with 21 health plans during fiscal year 2012–13, and it contracted with one additional health plan during fiscal year 2013–14 to raise the number to 22 health plans. However, Health Care Services performed medical audits of only five health plans in fiscal year 2012–13, 10 health plans in fiscal year 2013–14, and—as of May 2015—nine health plans in fiscal year 2014–15. Therefore, Health Care Services has not ensured that all health plans are complying with the provisions of their contracts to provide Medi‑Cal beneficiaries proper access to health care.
According to the chief of the Medical Review Branch, as of May 2015, his unit had six audit teams, each consisting of two medical consultants, two nurses, and two auditors. The audit teams also included one pharmacist, if available. He stated that all teams were fully trained and ready to meet the annual audit requirement. Further, he stated that his branch was in the process of developing a schedule of audits to be performed over the next fiscal year and that the goal is to fully meet the statutory annual audit requirement in fiscal year 2015–16.
Delays in Executing an Agreement Prevented Managed Health Care From Performing All Quarterly Assessments of Health Plans’ Provider Networks
Managed Health Care did not perform the quarterly assessments of provider network adequacy required under an agreement with Health Care Services. When these assessments are not completed, the State cannot be certain that the health plans are maintaining adequate provider networks to serve Medi‑Cal beneficiaries. The State has established patient access standards for health plans’ provider networks through regulations and contract provisions. In accordance with state law, Health Care Services enters into an agreement with Managed Health Care to review provider networks. As the Introduction discusses, Health Care Services entered into two agreements with Managed Health Care to perform quarterly reviews of provider network adequacy. The first agreement, signed in 2011, involved performing these assessments for the 30 counties that were participating in Medi‑Cal managed care at the time. The second agreement, signed in 2014, was for assessments for 28 additional counties after Medi‑Cal managed care expanded to rural counties. Although Managed Health Care confirmed that it assessed health plans serving all counties for the first quarter of 2014, since then it has been unable to perform the assessments of health plans serving the 28 counties that were part of the expansion of Medi‑Cal managed care to rural counties. The health plans in these counties had a total Medi‑Cal enrollment of nearly 351,000 as of March 2014 and more than 515,000 in March 2015.
Although the Legislature approved four limited‑term positions in June 2013 for July 2013 through December 2014, Managed Health Care stated that it did not fill these positions before their expiration in December 2014. The Legislature approved these positions for Managed Health Care to conduct adequacy assessments of provider networks for the Healthy Families Program’s transition to Medi‑Cal. According to the deputy director of Managed Health Care’s Office of Plan Licensing (licensing chief), the work performed for the transition was very similar to the work required under the agreement with Health Care Services. Therefore, Managed Health Care planned to use these same positions to perform the work outlined in the agreement. She stated that Managed Health Care waited to fill the positions until the agreement was signed. However, the departments did not sign this agreement until May 2014,and the California Department of General Services did not approve it until June 2014. At that point, according to the licensing chief, Managed Health Care decided not to spend resources trying to fill the limited‑term positions, given their impending expiration. Instead, its existing staff performed the reviews for the first quarter of 2014, but Managed Health Care determined that it could not sustain that amount of additional work. According to a senior attorney in the Office of Plan Licensing, the delays in executing the agreement were caused by several factors, such as multiple changes in the scope of the agreement, which resulted in additional reviews by Managed Health Care and Health Care Services’ Contract Management Unit. However, the licensing chief stated that because of a recent increase in staffing levels, as of May 2015, Managed Health Care plans to resume soon the quarterly reviews for all counties, beginning with reviews for the first quarter of 2015.
Managed Health Care Has an Opportunity to More Efficiently Fulfill Some of Its Monitoring Responsibilities That Overlap With Health Care Services
Both Managed Health Care and Health Care Services perform periodic reviews and audits of Medi‑Cal health plans using the standards established under the Knox‑Keene Act. Health Care Services must perform its audits of health plans more frequently than the reviews that Managed Health Care is required to perform. Therefore, we believe that Managed Health Care should rely on some of the work that Health Care Services performs as part of its audits.
State laws require both Health Care Services and Managed Health Care to perform periodic reviews of many health plans, including health plans for Medi‑Cal managed care. Specifically, state law requires Health Care Services to perform annual medical audits of each health plan for Medi‑Cal managed care to determine, among other things, the health plans’ ability to provide quality health care services and to assess the overall performance of the health plans in providing health care benefits to their enrollees. Another state law requires Managed Health Care to review at least once every three years all of the health plans it licenses, which include 17 of the 22 health plans for Medi‑Cal managed care. Managed Health Care’s review must include evaluations of the plans’ internal procedures for assuring quality of care and the overall performance of the plans in providing health care benefits and meeting the health needs of the enrollees.
As Table 5 below shows, the two departments’ reviews include many overlapping areas. For example, both Health Care Services and Managed Health Care review whether each health plan ensures that services are accessible and availableto enrollees within reasonable time frames and whether each health plan resolves all grievances and appeals in a professional, fair, and timely manner. In fact, Managed Health Care reviews only one area that Health Care Services does not review. Specifically, Managed Health Care reviews whether each health plan has implemented a language assistance program to ensure that interpretation and translation services are accessible and available to enrollees. Similarly, Health Care Services reviews one area that Managed Health Care does not. Health Care Services analyzes the administrative capacity and organizational structure of each health plan to make certain that it has both a full‑time medical director and a program in place to identify instances of fraud and abuse. Nevertheless, the two departments’ reviews overlap in seven areas.
| Area of Review | Description of Review | California Department of Health Care Services (Health Care Services) | California Department of Managed Health Care (Managed Health Care) |
|---|---|---|---|
| Utilization Management | Whether a California Medical Assistance Program (Medi‑Cal) managed care health plan (health plan) manages the utilization of services through a variety of cost‑containment mechanisms while ensuring access and quality care. | Reviewed | Reviewed |
| Access and Availability of Services | Whether a health plan ensures that its services are accessible and available to enrollees throughout its service areas within reasonable time frames. | Reviewed | Reviewed |
| Quality Management | Whether a health plan assesses and improves the quality of care it provides to its enrollees. | Reviewed | Reviewed |
| Grievances and Appeals | Whether a health plan resolves all grievances and appeals in a professional, fair, and expeditious manner. | Reviewed | Reviewed |
| Case Management and Coordination of Care | Whether a health plan ensures that services are furnished in a manner providing continuity and coordination of care and ready referral of patients to other providers consistent with good professional practice. | Reviewed | Reviewed |
| Administrative and Organizational Capacity | Whether a health plan has the administrative capacity and organizational structure to ensure compliance with contractual responsibilities, to ensure an independent medical decision-making process, and take appropriate corrective action against fraud, abuse, or both in the provision of health services under the Medi‑Cal program. | Reviewed | NOT REVIEWED |
| Language Assistance | Whether a health plan implements a language assistance program to ensure that interpretation and translation services are accessible and available to enrollees. | NOT REVIEWED | Reviewed |
| Access to Emergency Services and Payment* | Whether a health plan ensures that emergency services are accessible and available and that timely authorization mechanisms are provided for medically necessary care. | Reviewed | Reviewed |
| Prescription Drugs* | Whether a health plan that provides prescription drug benefits maintains an expeditious authorization process for prescriptions and ensures benefit coverage is communicated to enrollees. | Reviewed | Reviewed |
Sources: The website for Managed Health Care, a division overview document from Health Care Services, and the chief of the Medical Review Branch at Health Care Services.
* Health Care Services reviews these areas as part of the access and availability of services component of its review.
Although the two departments stated that they coordinate their efforts to a certain extent, the coordination focuses on minimizing their impact on the health plan. Specifically, staff from the two departments meet periodically to discuss the time frames for reviewing a health plan to ensure that they coordinate the timing of their reviews. According to the chief of Health Care Services’ Medical Review Branch, the two departments also coordinate their efforts to eliminate contradictions in their reports.
However, given the overlapping focus of the two departments’ reviews, Managed Health Care has an opportunity to reduce or eliminate duplication of work. State laws allow the two departments to rely on each other’s work to meet the statutory requirement, but neither department has done so. Because Health Care Services must review the 22 Medi‑Cal health plans more frequently than Managed Health Care, we believe that for the 17 Medi‑Cal health plans that it licenses, Managed Health Care should rely on Health Care Services’ reviews for information that falls under the review areas that overlap. This practice will allow Managed Health Care to focus its reviews of these health plans on the limited areas that Health Care Services does not review.
As stated earlier, Health Care Services began performing the required annual audits of health plans in 2012. Although Managed Health Care does not rely on the work performed by Health Care Services, the two departments havebeen coordinating since 2013 to minimize duplication of work. The deputy director of Managed Health Care’s Help Center stated that although Managed Health Care does not rely on the work performed by Health Care Services, the two departments are presently sharing audit tools, coordinating survey logistics, and sharing audit findings and corrective actions to minimize the amount of duplication that occurs. However, Managed Health Care can further reduce and potentially eliminate overlapping reviews of health plans by using, to the extent possible, the work performed by Health Care Services during its annual audits to fulfill Managed Health Care’s review requirement. Thedeputy director also stated that Managed Health Care is analyzing methods to use work performed during Health Care Services’ audits to meet the legal requirements for its future reviews of Medi‑Cal managed care plans. He statedthat Managed Health Care will assess Health Care Services’ annual audit processes and findings to better understand its methodologies before determining to what extent Managed Health Care can rely on Health Care Services’ work.
Recommendations
To ensure that Health Care Services accurately analyzes the adequacy of provider networks when initially certifying a health plan and when new beneficiary populations are added, it should establish by September 2015 a process to verify the accuracy of the provider network data that it uses to determine if a health plan meets adequacy standards for provider networks.
To make certain that it can provide support for its review process related to the adequacy of provider networks, Health Care Services should maintain for three years all documentation that supports its provider network certifications.
To ensure that Managed Health Care reaches accurate conclusions during its quarterly assessments of the adequacy of provider networks, Health Care Services should establish by September 2015 a process to verify the accuracy of the provider network data it receives from health plans and forwards to Managed Health Care. For example, Health Care Services could verify, for a sample of physicians claimed as part of the health plans’ provider networks, that health plans have current written agreements with the providers.
To improve the accuracy of provider directories, by December 2015 Health Care Services should revise its processes for monitoring health plans’ provider directories. Specifically, Health Care Services should review how each health plan updates and verifies the accuracy of the directory. In addition, Health Care Services should identify best practices and require the plans to adopt those practices.
To ensure that its review of provider directories is effective in identifying inaccurate information before it approves them for publication, Health Care Services should establish by September 2015 more detailed written policies and procedures for staff to follow that will provide evidence that staff are verifying the accuracy of provider directories. This verification process should include, at a minimum, the following elements:
- Developing a standard process for selecting a random sample, including procedures for selecting a sample size that is sufficient to identify errors in a provider directory and to enable Health Care Services to understand the accuracy of the entire directory. Health Care Services should then ensure that staff follow this process.
- Requiring staff to maintain for at least three years the documentation of their reviews and the verifications of the accuracy of provider directories.
- Retaining for three years Health Care Services’ communications with the health plans about any errors found in the directories or about the approvals of the directories.
- If Health Care Services finds significant errors in a health plan’s provider directory, it should work with that health plan to identify reasons for the inaccuracies and require the health plan to develop processes to eliminate the inaccuracies.
To ensure that it can handle adequately the volume of calls from Medi‑Cal beneficiaries, Health Care Services should implement an effective plan to upgrade or replace its telephone system and database to make certain that its ombudsman office can handle the volume of calls and maintain complete data to make informed management decisions. Further, after upgrading or replacing its systems, if Health Care Services believes that it does not have adequate staffing to address workload, it should justify its need and request additional staff.
To make certain that Health Care Services complies with state law requiring it to conduct annual medical audits, it should finish developing and begin adhering to its schedule for auditing all health plans in fiscal year 2015–16.
To ensure that Health Care Services complies with state law, it should increase its oversight of Managed Health Care to ensure that it completes the quarterly assessments required under the agreements. To make certain that Managed Health Carecomplies with its contractual obligations, it should continue its plan to perform quarterly reviews of the adequacy of provider networks beginning with the first quarter of 2015. Managed Health Care should monitor workload closely, and it should justify and request additional staff if it determines it does not have adequate staffing to perform quarterly reviews.
To increase the efficiency of statutorily required reviews by eliminating duplicative work, Managed Health Care should complete by September 2015 its planned assessment of the extent to which it can rely on Health Care Services’ annual audits. If it determines that Health Care Services’ work is sufficient to meet Managed Health Care’s responsibility under the Knox‑Keene Act, it should coordinate with Health Care Services to eliminate the duplication of work.
We conducted this audit under the authority vested in the California State Auditor by Section 8543 et seq. of the California Government Code and according to generally accepted government auditing standards. Those standards require that we plan and perform the audit to obtain sufficient, appropriate evidence to provide a reasonable basis for our findings and conclusions based on our audit objectives specified in the scope section of the report. We believe that the evidence obtained provides a reasonable basis for our findings and conclusions based on our audit objectives.
Respectfully submitted,
ELAINE M. HOWLE, CPA
State Auditor
Date:
June 16, 2015
Staff:
Tammy Lozano, CPA, CGFM, Audit Principal
Kris D. Patel
Jim Adams, MPP
Ryan T. Canady
Chuck Kocher, CIA, CFE
Legal Counsel:
Joseph L. Porche, Staff Counsel
For questions regarding the contents of this report, please contact Margarita Fernández, Chief of Public Affairs, at 916.445.0255.
Footnotes
5 The Healthy Families Program provided health, dental, and vision coverage to uninsured children who did not qualify for no‑cost Medi‑Cal. Go back to text