Department of Health Care Services and Department of Managed Health Care
Children Enrolled in Medi‑Cal Face Challenges in Accessing Behavioral Health Care
November 28, 2023
2023-115
The Governor of California
President pro Tempore of the Senate
Speaker of the Assembly
State Capitol
Sacramento, California 95814
Dear Governor and Legislative Leaders:
As directed by the Joint Legislative Audit Committee, my office conducted an audit of the Department of Health Care Services (DHCS) and the Department of Managed Health Care (Managed Health Care). Our assessment focused on access to behavioral health services for children in Medi-Cal, and the following report details the audit’s findings and conclusions. In general, we determined that the departments can do more to detect and address challenges that children face when seeking behavioral health services.
Survey results of appointment wait times show that many Medi-Cal managed care plans are unable to provide children with timely access to behavioral health care. However, we also found that certain weaknesses in the way DHCS and Managed Health Care conduct the surveys and report on the results limit the surveys’ effectiveness at conveying the true extent of timely access issues. Further, data from DHCS’ monitoring of specialty mental health plans show that a significant number of counties are also out of compliance with applicable standards for timely access.
Our review also found that DHCS must make improvements to the way it monitors the capacity of Medi-Cal managed care plans to provide services for their members. For example, DHCS approves potentially unreasonable standards for the time and distance Medi-Cal members must travel to see behavioral health care providers. Furthermore, the department’s enforcement activities do not always ensure that a plan takes steps to meaningfully improve access.
To address our findings, we make several recommendations, including that DHCS and Managed Health Care make changes to the methodology of their timely access surveys to monitor compliance with the standards for the most urgent appointment types and then to disclose the proportion of providers excluded from survey results along with the reasons for those exclusions. We also recommend that DHCS revise its agreements with managed care plans to require them to demonstrate efforts to recruit new providers to underserved areas and to implement a policy outlining when noncompliance with standards justifies financial penalties.
Respectfully submitted,
GRANT PARKS
California State Auditor
Selected Abbreviations Used in This Report
| CAP | corrective action plan |
| CCS | California Children’s Services |
| CDC | Centers for Disease Control and Prevention |
| CMS | Centers for Medicare & Medicaid Services |
| DHCS | Department of Health Care Services |
| DMC | Drug Medi‑Cal Treatment Program |
| DMC‑ODS | Drug Medi‑Cal Organized Delivery System |
Summary
Results in Brief
The Department of Health Care Services (DHCS) and the Department of Managed Health Care (Managed Health Care) can do more to detect and address challenges that children in Medi‑Cal face when seeking behavioral health services. Behavioral health care includes care for both mental health and substance use issues, and research indicates that timely access to this care is critical. State law provides that timely access is the allowable time frame by which a health care service plan must offer appointments to members. Though there are no statewide data to demonstrate precisely how long it takes Medi‑Cal patients to receive behavioral health care once they request it, survey data for appointment wait times show that many Medi‑Cal managed care plans are unable to provide timely access for children. For example, 43 percent of urgent appointments with psychiatrists DHCS surveyed in 2022 exceeded the 96‑hour appointment wait time standard, and the median wait time for those appointments was almost 13 days.
Both DHCS and Managed Health Care play a role in monitoring managed care plans to ensure that the plans are meeting timely access standards, but weaknesses in the way they conduct this monitoring limit its effectiveness. DHCS and Managed Health Care oversee surveys of providers to determine how long it takes for members to get appointments, but the surveys are not always specific to children and do not measure whether plans’ providers meet the standards for urgent appointments with the shortest allowable wait time of just 48 hours. Further, DHCS and Managed Health Care exclude from the compliance rates they publish health care providers who do not respond to the survey or for whom they have incorrect contact information. For example, Managed Health Care’s data indicate that about 30 percent of surveyed therapists were excluded from its 2021 survey results because, among other possible reasons, they were deemed ineligible because of incorrect provider information or provider non‑responsiveness. It would be reasonable to exclude providers who do not respond from those specific calculations, however, the departments should find other ways to communicate this information to users of the surveys so those users are aware of potential issues contacting providers in a given plan. Because the surveys do not currently do this, the resulting reports may not sufficiently represent the plans’ capacities to serve patients: plan members who face difficulties in reaching a provider because of incorrect contact information or unresponsiveness may experience access challenges for which the survey results do not account.
The results of DHCS’ timely access monitoring of specialty mental health care and substance use treatment plans administered by counties similarly show that significant numbers of counties’ plans are not in compliance with DHCS’ standards. For children, the consequences of delays in access to behavioral health services can be serious. Some health care groups report that untreated mental health disorders can negatively affect a child’s healthy development and lead to severe consequences, including suicide. In our review of 54 medical records of children who likely faced delays in accessing behavioral health services, we found three instances in which the records indicated a worsening of children’s conditions from a lack of care, including one instance in which the child required hospitalization.
In addition to weaknesses in its survey methodologies, our review found that DHCS needs to make improvements to the way it monitors network adequacy, which is a Medi‑Cal managed care plan’s capacity to provide services to its members. For example, despite clear indications of provider shortages, flaws in how DHCS calculated the minimum provider‑to‑member ratios it requires plans to meet led it to conclude that every managed care plan had at least 80 times as many pediatric non‑specialty mental health care providers as DHCS required, and five of the 24 plans had more than 1,000 times as many providers as required. In contrast to DHCS’ approach, our review found that it is more relevant to consider the number of services a provider delivers to Medi‑Cal members than to simply count the number of providers available to provide services to those enrolled in Medi‑Cal.
DHCS also continues to approve potentially unreasonable standards for the time and distance Medi‑Cal members must travel to see behavioral health care providers in managed care plans. In 2022 DHCS approved 40 alternative access standards for providers like psychologists and therapists that can require children to travel two hours or more to receive care in some, generally rural, areas of the State. Furthermore, the department’s enforcement activities do not always ensure that a plan takes steps to meaningfully improve access. When plans fail to meet standards, DHCS can impose a corrective action plan (CAP) on the managed care plan or county mental health plan to remedy the deficiencies. However, our review of recent CAPs found that they typically only resulted in managed care plans submitting missing or corrected documentation and did not address the underlying causes of long or unequal distances members must travel. DHCS could more meaningfully increase access to care if it improved its review of network adequacy and held deficient plans accountable by requiring them to cover out‑of‑network services for the members affected by standards that could require them to travel unreasonable or inconsistent distances for care. Further, because of challenges posed by the COVID‑19 pandemic, DHCS typically has not issued any sanctions or other penalties for managed care plans or county mental health plans that fail to completely follow their CAPs. Without making needed improvements to how it monitors managed care plans’ network adequacy, and then issuing sanctions when warranted or taking other actions to increase the impacts of its oversight, DHCS is missing opportunities to ensure that qualifying children receive the behavioral health care services to which they are entitled.
Agency Comments
DHCS indicated that it would implement our recommendations, and described actions it has already taken or plans to take to address some of the issues we identify in the report. Although Managed Health Care indicated that it appreciated our recommendations, it indicated that implementing them would require the Legislature to grant it an extension to its exemption from the Administrative Procedure Act in order to test and refine changes to its timely access survey methodology.
Introduction
Background
The Growing Crisis Related to Children’s Mental Health
In 2021 the American Academy of Pediatrics, the American Academy of Child and Adolescent Psychiatry, and the Children’s Hospital Association jointly declared a state of emergency in child and adolescent mental health. As potential evidence of what those groups called a “worsening crisis,” the Centers for Disease Control and Prevention (CDC) has reported on academic research concluding that more than one in five children ages 13 to 18 currently have or have had a seriously debilitating mental illness. The CDC reports that mental health disorders present serious challenges in the way children typically learn, behave, and handle their emotions, and that some common mental health disorders diagnosed in children include anxiety, depression, and attention‑deficit/hyperactivity disorder.
Behavioral Health, which is sometimes called mental health, often includes substance use. For the purpose of this audit, we refer to programs and treatment for mental health and substance use disorders as behavioral health care. The consequences for children who do not receive necessary behavioral health care can be potentially severe. According to the CDC, undiagnosed and untreated mental health disorders in children can lead to problems at home, in school, and in forming friendships. Nearly 21 percent of children in California did not receive needed mental health care in 2021 and 2022, according to a report by the Commonwealth Fund, which ranked the State of California as 38th in the nation for that metric.The Commonwealth Fund is a private foundation that publishes an annual report on states’ health systems called the Scorecard on State Health System Performance. The National Alliance on Mental Illness states that untreated mental health conditions can result in poor quality of life, substance abuse, unemployment, and suicide, among other negative outcomes. According to the CDC, suicide is the second leading cause of death for children and young adults between the ages of 10 and 24. Conversely, the World Health Organization reports that promoting mental health and preventing mental health issues enhances an individual’s mental well‑being and resilience, and increasing evidence demonstrates that such measures are also cost‑effective.
Access to Behavioral Health Care for Children in Medi‑Cal
Reported Demographics of Medi-Cal and California Populations
| Ethnicity | Percentage of Certified Eligible Medi-Cal Beneficiaries As of November 2022 |
Percentage of California’s population As of July 2022 |
| Hispanic* | 48 | 40 |
| White | 17 | 35 |
| Asian or Pacific Islander | 9 | 17 |
| Black | 7 | 7 |
| Alaskan Native or American Indian | >1 | 2 |
| Not Reported | 18 | N/A |
Source: DHCS’ Medi-Cal at a glance, November 2022 data and population estimates from the U.S. Census Bureau.
* The U.S. Census uses the category Hispanic or Latino rather than Hispanic, and notes that people in this category can be included in other categories as well.
Medi‑Cal is the State’s Medicaid program and offers health care coverage for eligible Californians, both children and adults. As of November 2022, 15.5 million Californians were enrolled in Medi‑Cal. The text box shows the demographic composition of certified eligible Medi-Cal beneficiaries compared to the population of the State as a whole as of 2022. As of December 2022, about 5.7 million of the Californians enrolled in Medi‑Cal were younger than the age of 21. As Figure 1 shows, the State provides behavioral health services to Medi‑Cal members through various delivery systems, which include managed care, fee‑for‑service, and services administered by counties. The Department of Health Care Services (DHCS) also classifies members’ needs for mental health care into two categories: those requiring specialty mental health services and those requiring non‑specialty mental health services.
Figure 1
Children in Medi‑Cal Access Behavioral Health Care Through Multiple Delivery Systems
Source: State law and DHCS.
Figure 1 description:
This figure presents the three different behavioral health care delivery systems and which services they provide. There are icons representing all three systems, with arrows pointing to text describing the find of services can be delivered through those systems. The Managed Care and Fee-For-Service icons have arrows that merge, pointing to text that reads "Managed Care and fee-for-service providers deliver non-specialty mental health services, such as individual therapy." The "counties" delivery system icon points to text that reads "Counties cover specialty mental health services, such as acute inpatient psychiatric treatment, and substance use treatment." The words "non-specialty", "specialty", and "substance use treatment" are bolded.
Examples of non‑specialty mental health services include individual and group therapy, psychiatric consultation, and psychological testing. Children in Medi‑Cal receive non‑specialty mental health services through a managed care plan or a fee‑for‑service provider. A Medi‑Cal managed care plan covers basic medical benefits and provides members with a network of providers, pharmacies, clinics, and hospitals. DHCS pays the managed care plan a monthly rate for each Medi‑Cal member enrolled in that plan, and the managed care plan maintains a network of providers to deliver services to its members. As Figure 2 shows, 95 percent of all children in Medi‑Cal were enrolled in a managed care plan as of December 2022. Some children, such as those who are new to Medi‑Cal and have not yet enrolled in a managed care plan, are covered under the fee‑for‑service system. In this system, providers render services and then submit claims for payment.
Figure 2
Most Children Enrolled in California Children's Services Are Also in Medi‑Cal Managed Care
Source: DHCS’ 2022 Medi‑Cal Children’s Health Dashboard and California Children’s Services enrollment data.
Figure 2 description:
This figure is comprised of a tan colored circle with a thick red outline and a smaller overlapping blue circle with the majority of that smaller circle inside the larger circle. Blue text below the smaller overlapping circle describes the smaller circle by stating "195,000 children are enrolled in California Children's Services”. Below that is clip art of five children. Below the clip art of children, red text describes the larger circle by stating “5,700,000 children are enrolled in Medi-Cal”. There is an arrow that points to the inside of the larger circle stating "95% of children enrolled in Medi-Cal are in managed care plans." There is an arrow that points to the thick red outline of the larger circle that says "5% are in Medi-Cal Fee-For-Service." The smaller blue circle that lays on top of the other circle has a portion on top that both overlaps the thick red outline of the larger circle and reaches above the larger circle. This portion is colored a lighter blue than the potion of the smaller circle that is inside of the tan larger circle. There is an arrow that points to the darker blue portion of the smaller circle, the portion that is inside the tan larger circle that says "90% of children in California Children's Services are in Medi-Cal Managed Care." There is an arrow that points to the light blue portion of the circle that overlaps a small portion of the red border of the tan circle at the top and extends slightly above the border that says "10% have other health coverage."
Children who meet access criteria for specialty mental health services may receive the broad array of services that are available through county mental health plans. Access criteria for specialty mental health services include children suffering from a significant impairment due to a diagnosed mental disorder and children at high risk of developing mental disorders due to experiences of trauma or involvement in the child welfare or juvenile justice system. In addition to services like individual and group therapy that may also be covered as non‑specialty mental health services, specialty mental health services include psychosocial rehabilitation services that provide assistance in restoring, improving, or preserving a beneficiary’s functional, social, or daily living skills. Specialty mental health services also include more intensive services like acute inpatient psychiatric treatment, crisis residential treatment services, crisis intervention and stabilization, and intensive care coordination. Counties deliver Medi‑Cal specialty mental health services through their own county mental health plan, and they deliver Medi‑Cal substance use treatment programs through the Drug Medi‑Cal Treatment Program or Drug Medi‑Cal Organized Delivery System (Drug Medi‑Cal programs). A Medi‑Cal beneficiary may receive both non‑specialty and specialty mental health services at the same time, as long as the beneficiary meets the criteria for both non‑specialty and specialty mental health services and the services are clinically appropriate, coordinated, and not duplicative. According to DHCS, during fiscal year 2020–21, approximately 244,000 individual children—or about 5 percent of all children enrolled in Medi‑Cal that year—obtained specialty mental health services.
DHCS, in conjunction with county health departments, administers the California Children’s Services (CCS) program, which provides medical treatment to children younger than the age of 21 with certain chronic physical conditions such as cerebral palsy, heart disease, or cancer. To qualify for CCS, a child with a CCS‑eligible condition must be either already enrolled in Medi‑Cal, have family income of less than $40,000, or have anticipated out‑of‑pocket medical expenses greater than 20 percent of family income. Although CCS may cover services for mental health issues if the underlying condition is a complication of the CCS‑eligible condition or interferes with the medical treatment of the CCS‑eligible condition, state law generally excludes mental health issues from CCS‑eligible conditions. Therefore, children enrolled in CCS would generally receive behavioral health services through other health coverage programs, such as private insurers or Medi‑Cal. As Figure 2 shows, approximately 195,000 children in the State were enrolled in CCS as of December 2022, and about 90 percent of those children were also enrolled in a Medi‑Cal managed care plan.
Oversight of Behavioral Health Care for Children in Medi‑Cal
The Centers for Medicare & Medicaid Services (CMS) administers the federal Medicaid program. Federal law establishes the general rules that all state‑run Medicaid programs must follow, but it allows CMS to grant states flexibility in the administration of state programs and the delivery of care. For instance, federal law requires all states to provide certain mandatory benefits, including inpatient and outpatient hospital services, but it allows states to decide whether to cover optional benefits, such as prescription drugs and hospice care.
Federal law requires states to designate a single state agency to administer the State’s Medicaid program. DHCS administers Medi-Cal in California. In this role, DHCS is responsible for creating and overseeing policies and regulations for the State’s Medicaid program, including setting payment rates. DHCS also contracts with managed care plans to provide coverage to Medi‑Cal members.
California’s law known as the Knox‑Keene Health Care Service Plan Act of 1975 (Knox‑Keene Act) generally requires health care service plans, including those that contract to serve as Medi‑Cal managed care plans, to obtain a license in order to provide coverage for the State’s residents. The Department of Managed Health Care (Managed Health Care) regulates all health care service plans licensed under the Knox-Keene Act. As a result, both DHCS and Managed Health Care are responsible for overseeing most Medi‑Cal managed care plans: DHCS as the administrator of Medi‑Cal and contractor with Medi‑Cal managed care plans, and Managed Health Care as the regulatory body overseeing Knox‑Keene licensees. However, Managed Health Care does not oversee county mental health plans and Drug Medi‑Cal programs, because it has determined that they do not meet the definition of a health care service plan under the Knox‑Keene Act. As such, only DHCS oversees county mental health plans and Drug Medi‑Cal programs. Figure 3 summarizes the monitoring responsibilities of DHCS and Managed Health Care.
Figure 3
DHCS and Managed Health Care Monitor Timely Access for Certain Health Plans and Programs
Source: State law and DHCS and Managed Health Care documentation.
* State law exempts county organized health systems (COHS) from the Knox‑Keene Act for purposes of carrying out Medi‑Cal contracts. According to Managed Health Care, Health Plan of San Mateo is the only COHS that has voluntarily obtained a Knox‑Keene license for its Medi‑Cal line of business.
† Timely access standards in state law apply to health care service plans and Medi‑Cal managed care plans; DHCS confirmed that those timely access standards do not apply to the Medi‑Cal fee‑for‑service delivery system it oversees.
Figure 3 description:
This figure has two boxes showing which health plans and programs have timely access monitored by DHCS and Managed Health Care. Above each of the two boxes are clip art images of stethoscopes. On the left, the box says "DHCS monitors timely access for all Medi-Cal managed care plans, all county mental health plans, and all Drug Medi-Cal and Drug-Medical Organized Delivery Systems." On the right, the box says "Managed Health Care monitors timely access for all health care service plans with a Knox-Keene license. This currently includes the majority of, but not all, Medi-Cal managed care plans." There is an asterisk at the end of the sentence that points to a note that reads "State law exempts county organized health systems (COHS) from the Knox-Keene Act for purposes of carrying out Medi-Cal contracts. According to Managed Health Care, Health Plan of San Mateo is the only COHS that has voluntarily obtained a Knox-Keene license for its Medi-Cal line of business." Below both boxes is text that reads "Neither DHCS nor Managed Health Care monitor timely access for Medi-Cal fee-for-service. There is a cross at the end of the sentence that points to a note that reads "Timely access standards in state law apply to health care service plans and Medi-Cal managed care plans; DHCS confirmed that those timely access standards do not apply to the Medi-Cal fee-for-service delivery system it oversees.
Timely Access Standards for Behavioral Health Care Appointments in California
Federal law requires each state to ensure that all services covered by Medicaid are available to managed care members in a timely manner. In California, state law requires Medi‑Cal managed care plans, county mental health plans, and certain substance use programs to follow the timely access standards set for health care service plans in the State through the Knox‑Keene Act. State law provides that timely access is an established allowable time frame by which a plan must offer its members appointments. For example, a Medi‑Cal managed care plan must be able to offer its members a non‑urgent mental health appointment with a psychologist within 10 days of the request for an appointment.
Both DHCS and Managed Health Care play a role in monitoring health plans to ensure that the plans are meeting timely access standards. For Medi‑Cal managed care plans, both DHCS and Managed Health Care oversee surveys to monitor plans’ compliance with timely access standards. The surveyors contact providers that participate in the plans’ provider networks, notify the providers of the purpose of the survey, and ask the providers for the date of the soonest available appointment. If a plan is not in compliance with timely access standards, DHCS and Managed Health Care can require the plan to take corrective action or face financial sanctions. In the last four years, DHCS has also begun requiring county mental health plans and county substance use treatment programs to submit real patient data about how long it takes members to access an appointment. According to DHCS’ oversight section chief (section chief), fiscal year 2022–23 was the first year that the department collected data from county mental health plans and county substance use treatment programs for children as a specific group.
Audit Results
Available Data Substantiate Long Wait Times to Access Behavioral Health Care for Many Children in Medi‑Cal
Despite a lack of statewide data that demonstrate precisely how long it takes patients in California to receive behavioral health care, information collected by the Department of Health Care Services (DHCS) and the Department of Managed Health Care (Managed Health Care) through surveys indicate that many Medi‑Cal managed care providers are unable to provide timely care. That same information also shows that the availability of timely care varies, sometimes significantly, based on the managed care plan (plan), geography, and type of appointment. Furthermore, we identified several weaknesses in the methods DHCS and Managed Health Care use to collect appointment timeliness information. These weaknesses may lead to an overestimation of the availability of timely appointments statewide and limit the usefulness of the resulting data on timely care. Additionally, DHCS can do more to ensure that county mental health and substance use treatment plans also abide by the timely access standards in state law.
Survey Results Indicate Significant Access Issues in Many Medi‑Cal Managed Care Plans in Different Parts of California
In assessing the availability of data on timely access to behavioral health care in California, we found that neither DHCS nor Managed Health Care collect statewide data about how long patients wait for requested appointments and instead monitor timely access by other means. Both departments assert that collecting this specific data would not be feasible. According to the director of Managed Health Care, the software programs that providers use do not capture the data elements that the department would need to assess appointment wait times. At minimum, Managed Health Care indicated that it would need providers’ software to capture provider and appointment type as well as the dates of request for the appointment, first offered appointment, and scheduled appointment. According to the DHCS Director’s Office, a requirement to collect this data would be more complex and costly for DHCS and providers than current practices. The absence of this specific data in California does not appear to be unusual. In our review of 12 other states’ practices, we did not identify evidence of any state collecting specific wait time information or requiring providers and plans to do so. Further, the academic research and federal guidance we reviewed does not mention collecting this data as an element of best practices for monitoring timely access compliance. Instead, the federal Centers for Medicare & Medicaid Services (CMS) has issued a proposed rule that would require conducting surveys in which the surveyor poses as a member to evaluate plan compliance with appointment wait time standards in order to add validity and accuracy to states’ efforts to measure access to services.
Instead of collecting statewide data for actual appointment wait times, both DHCS and Managed Health Care oversee surveys of providers to evaluate plans’ compliance with the timely access standards in law that establish maximum allowable wait times for patients requesting various types of health care. To administer its survey, DHCS uses an external quality review organization to contact a statistically significant number of providers of each relevant type—411 providers in 2022—and request information about the earliest available appointments. Managed Health Care has also implemented a standardized methodology for plans to either annually survey statistically reliable samples of their own contracted providers, or to use an external vendor to do so.We discuss specific elements of the departments’ survey methodologies in the following section. The surveys cover various types of providers, two of which are applicable to behavioral health care: non‑physician mental health care providers (therapists), such as psychologists and licensed clinical social workers; and psychiatrists, which are included in the broader specialist category in DHCS’ survey. As Table 1 illustrates, there are different timely access standards for various types of urgent and non‑urgent appointments.
Table 1
State Law Requires Plans to Have Enough Providers to Allow Members to Receive Appointments Within Established Acceptable Wait Times
| Appointments | Time Frame |
| Urgent | |
| Services that do not require prior authorization | 48 hours |
| Services that do require prior authorization | 96 hours |
| Non-Urgent | |
| Appointments with a therapist | 10 business days |
| Appointments with specialist physicians, including psychiatrists | 15 business days |
Source: State Law and DHCS and Managed Health Care documentation.
Note: A time frame for a particular appointment may be extended if the health care provider has noted that a longer wait time will not have a detrimental impact on the health of the member.
DHCS and Managed Health Care do not currently use timely access survey results to hold plans accountable through a standardized minimum level of performance across plans. According to state law, the purpose of the surveys is to evaluate a plan’s ability to offer appointments within the timely access standards. The standards require plans to have enough providers to offer enrollees appointments that meet the timely appointment standards; however, they do not require that every individual provider always be able to offer an appointment within the standards. Thus, Managed Health Care has adopted a threshold that it will use to evaluate its survey results in 2024, whereby 70 percent of providers surveyed within a given plan must offer appointments that meet the timely access standards. Managed Health Care says that it established the 70 percent threshold based on calculations determining that at this threshold, a member of the plan is likely to obtain a timely appointment by contacting no more than three different providers. Managed Health Care asserts that if plans fail to meet the 70 percent compliance standard in the survey results, the department will require the plans to investigate and submit a corrective action plan (CAP) and the plan may be subject to disciplinary actions, such as financial sanctions. For its own timely access survey, DHCS does not have a current threshold for therapists, but it has an 80 percent threshold for primary care providers and specialists. According to DHCS, the department has not established compliance thresholds for therapists because it is anticipating federal requirements. Nonetheless, until the departments apply a threshold specific to these providers, survey results will have limited utility as a means of ensuring timely mental health care access to all Medi‑Cal members.
In its own attempt to implement measurement thresholds for timely access, CMS has issued a proposed rule that, if adopted, could subject Medi‑Cal plans to a 90 percent compliance threshold for most providers. In response to the proposed rule, DHCS suggested that CMS should allow states to establish their own compliance thresholds to allow for alignment of appointment wait time standards across Medicaid delivery systems and commercial health care services. Regardless, as part of its duty to evaluate whether Medi‑Cal plans are providing members with timely access to mental health services, DHCS should implement a threshold based on a clear and reasonable expectation about what plans must ensure for their members.
DHCS’ 2022 results from its Medi‑Cal plan survey for therapists treating children suggest that many members face significant challenges in accessing timely appointments and that many plans’ providers cannot offer appointments within the legally required time frames. For example, only 63 percent of surveyed therapists in the California Health and Wellness plan could offer an appointment within the 10‑business day standard for non‑urgent appointments. Further, while state law allows just 48 hours for urgent appointments for services that do not require prior authorization, which generally includes appointments with therapists in Medi‑Cal plans, only 39 percent of the plan’s therapists could offer an urgent appointment within 96 hours.As discussed later in the report, DHCS currently measures appointments subject to the 48 hour requirement against a 96 hour standard but agrees it should change this practice. Plans throughout the State were generally even less able to provide timely urgent appointments than non‑urgent appointments. Figure 4 shows some examples of plans and the frequency with which they could offer timely appointments.
Figure 4
Many Medi‑Cal Therapists in a Selection of Health Plans Were Unable to Provide Children With Timely Appointments
Source: DHCS’ 2022 Medi‑Cal Timely Access Survey Data and Medi‑Cal Managed Care External Quality Review Technical Report.
Note: The percentage presented for each plan is the percentage of non‑urgent and urgent appointments available within timely access standards during DHCS’ timely access survey. The percentages only include the survey results for therapists and are measured against a standard of 10 business days for non‑urgent appointments and 96 hours for urgent appointments. As we discuss later, DHCS’ use of the 96 hour urgent appointment standard for all therapist appointments is incorrect. Enrollment totals are as of June 2022. See Appendix A for every plan’s results.
To view a larger version of Figure 4, please click on the above image.
Figure 4 description:
This figure contains the results of DHCS' 2022 timely access survey for 5 different Medi-Cal managed care plans. It is a figure with 5 plans on the vertical axis. The horizontal axis has percentages from 0-100 in 10% increments and is labeled with text saying "Percent of Appointments Available Within Timely Access Standards. There is a red dotted line at 90% that is labeled with text that says "Proposed Federal Standard." Each plan has two bars. One bar is blue, indicating the results for non-urgent appointments. The other bar is orange, indicating the results for urgent appointments. The first plan is labeled "San Francisco Health Plan (162,000 enrollees)." The non-urgent bar is at 99.6% and the urgent bar is at 98.8%. The second plan is labeled "Kaiser (193,000 enrollees)." The non-urgent bar is at 93.5% and the urgent bar is at 75.3%. The third plan is labeled "CalViva Health (407,000 enrollees)." The non-urgent bar is at 76.9% and the urgent bar is at 58.4%. The fourth plan is labeled "California Health and Wellness Plan (233,000 enrollees)." The non-urgent bar is at 63.2% and the urgent bar is at 39.3%. The fifth plan is labeled "United Healthcare Community Plan (30,000 enrollees)." The non-urgent bar is at 25.1% and the urgent bar is at 0.0%. There is a note that reads "The percentage presented for each plan is the percentage of non-urgent and urgent appointments available within the timely access standards during DHCS' timely access survey. The percentages only include the survey results for therapists and are measured against a standard of 10 business days for non-urgent appointments and 96 hours for urgent appointments. As we discuss later, DHCS' use of the 96 hour urgent appointment standard for all therapist appointments is incorrect. Enrollment totals are as of June 2022. See Appendix A for every plan's results."
Overall, the median appointment wait time for children was about three days for all behavioral health care appointment types and providers, regardless of the applicable standard. However, as Figure 5 shows, when the earliest available appointment exceeded the applicable standard, which occurred about half the time for urgent appointments with therapists and psychiatrists alike, that appointment was sometimes months away. For example, 26 percent of non‑urgent appointments with therapists exceeded the 10‑business day timely access standard. Among the appointments that exceeded that timely access standard, the median wait time was 23 days, and some appointments were not available for 100 days or longer. In another example, 43 percent of urgent appointments with a psychiatrist exceeded the 96 hour timely access standard against which DHCS measures, and the median wait time for the appointments that exceeded that standard was almost 13 days.
Figure 5
Phone Call Surveys Showed a Wide Variance in Times for the Next Appointment for Children
Source: DHCS’ 2022 Medi‑Cal Timely Access Survey Data.
Note: Each dot represents a surveyed provider’s next available appointment time and does not represent a specific managed care plan’s average appointment time.
Figure 5 description:
This figure consists of many dots representing a provider's next available appointment time. There are 4 categories of different provider and appointment types indicated on the vertical axis and the number of days until the next available appointment, 0-150 days in 25 day increments, is indicated on the horizontal axis. In each entry, a vertical dotted red line indicates that the median appointment wait time and a vertical solid black line indicates that the appointment wait time standard. The first entry is labeled "Psychiatrist - Urgent. 19 of 44 (43%) of appointment times exceeded the 96 hour standard." 19 dots for this entry are clustered around 1-4 days, and 25 dots indicating the longer wait times are much more sporadic until the farthest dot, which indicates a wait time of about 93 days. The vertical dotted red line indicates that the median appointment wait time is about 4 days. The next entry is labeled "Psychiatrist - Non-Urgent. 8 of 47 (17%) of appointment times exceeded the 15-business day standard." The dots are clustered around 2 days, and then get more and more sporadic until the farthest dot indicates a wait time of about 70 days. The median appointment wait time was about 5 days. The third entry is labeled "Therapist - Urgent. 322 of 559 (58%) of appointment times exceeded the 48 hour standard." The dots are clustered tightly from about 0-10 days, and then get more and more sporadic until the farthest dot indicates a wait time of about 151 days. The median appointment wait time was about 3 days. The fourth entry is labeled "Therapist - Non-Urgent. 157 of 610 (26%) of appointment times exceeded the 10-business day standard." The dots are clustered tightly from 1-12 days, and then get more and more sporadic until the the farthest dot indicates a wait time of about 124 days. The median appointment wait time was about 3 days. There is a note that reads "Each dot represents a surveyed provider's next available appointment time and does not represent a specific managed care plan's average appointment time.
Managed Health Care’s survey results from 2021, the most recent year available at the time of our review in September 2023, similarly confirm that Medi‑Cal plans struggle to meet the timely access standards for behavioral health appointments. Managed Health Care monitors plans for each health care plan network (by county) in which a given plan operates. For non‑urgent appointments with therapists, roughly two‑thirds of the networks currently meet the 70 percent threshold that Managed Health Care has implemented. However, only 30 percent meet the threshold for offering timely urgent appointments. Similar to those from DHCS’ monitoring, these survey results indicate that members requiring urgent behavioral health care may be at particular risk of access barriers, which could result in worsening symptoms or other negative outcomes.
Access to timely behavioral health services through Medi‑Cal managed care plans can vary significantly by geographic area. DHCS’ survey results indicate that members in certain areas of the State may face greater access challenges than those in other areas, and the disparity in access sometimes exists even among counties within the same plan. For example, 60 percent of surveyed therapists in the Medi‑Cal Central California Alliance for Health plan were able to offer appointments within the 10‑business day non‑urgent standard in the Monterey/Santa Cruz region, but only 24 percent of the plan’s therapists in Merced County could do so.
Similarly, our analysis of behavioral health services provided statewide found wide variation in the average number of services children in Medi‑Cal actually received in 2022.Our analysis defined “behavioral health services” as Medi‑Cal claims for which behavioral health was the principal condition requiring medical attention. Even though each visit can consist of multiple individual procedures that are collectively reported to DHCS on a single claim, we counted each claim as one service. Figure 6 depicts the average number for each county in the State that year. For example, there was about one service provided per enrolled child in Madera County, compared to about three and a half services provided per enrolled child in Mendocino County. DHCS affirmed that regional disparities in access to behavioral health services is an issue, and there is room to improve, but the department noted that it would need to perform additional research on the topic to understand the scope of the issue as it relates to Medi‑Cal. When we shared the results of our analysis, DHCS responded that, among other factors, these differences could be due to more pronounced shortages of providers in rural areas as well as regional differences in opinion about the usefulness of behavioral health care. DHCS told us that its Managed Care Quality and Monitoring Division had not previously done analysis on regional differences in the number of behavioral services per child, but it is beginning to increase overall monitoring of networks to help decrease regional disparities in access to mental health services.
Figure 6
The Average Number of Delivered Behavioral Health Services per Beneficiary in Some Counties During 2022 Was More Than Triple the Average in Others
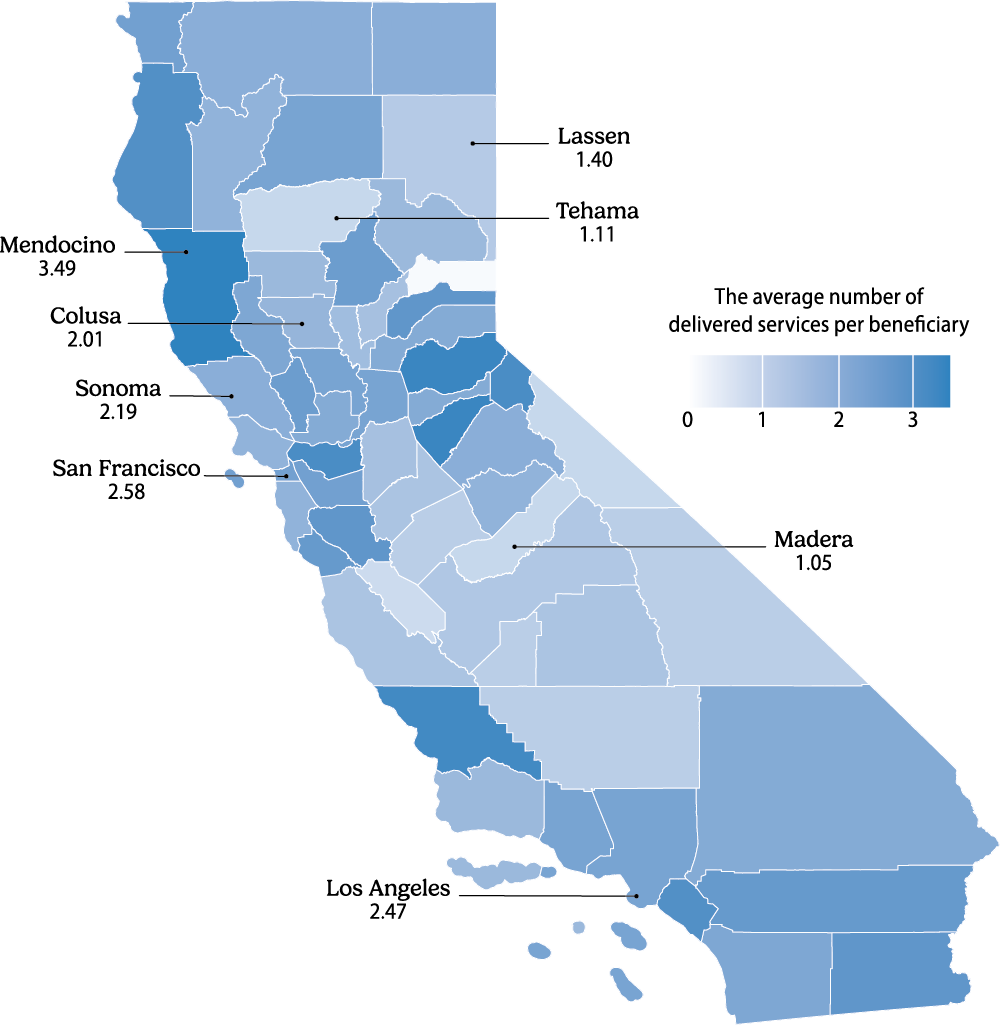
Source: DHCS Claims Data.
Note: Our analysis defined behavioral health services as Medi‑Cal claims where behavioral health was the principal condition requiring medical attention. While each encounter can consist of multiple procedures that are collectively reported to DHCS on a claim, we counted each claim as one service. The results for all counties are located in Appendix B.
Figure 6 description:
This figure shows a map of California with each county colored with a gradient ranging from white to dark blue indicating the average number of delivered behavioral health services per beneficiary. There is a legend labelled “The average number of delivered services per beneficiary showing the color gradient going from very light blue to dark blue along a scale of zero to about three and a half services per beneficiary. There is not an obvious pattern to the gradients other than the larger counties in central California appearing to be lighter colored than average. Several counties' results are highlighted and read as follows: "Lassen 1.40" "Tehama 1.11" "Mendocino 3.49" "Colusa 2.01" "Sonoma 2.19" "San Francisco 2.58" "Madera 1.05" and "Los Angeles 2.47." There is a note that reads "Our analysis defined behavioral health services as Medi-Cal claims where behavioral health was the principal condition requiring medical attention. While each encounter can consist of multiple procedures that are collectively reported to DHCS on a claim, we counted each claim as one service. The results for all counties are located in Appendix B."
Both departments acknowledge that their timely access survey results show that general availability of appointments could improve for some plans, and DHCS agreed that the results indicate that plans in certain parts of the State face challenges meeting compliance with required timely access standards. According to Managed Health Care, the department has not analyzed the timely access results in a way that isolates only mental health care access or such access for children in general. Managed Health Care separately stated that when looking at the results for all provider types surveyed by a health plan, including primary care physicians, the 2021 results show that most health plans met a 70 percent or greater compliance threshold for non‑urgent appointments and many did so for urgent appointments. However, our analysis of Managed Health Care’s survey results specifically for therapists and psychiatrists shows significant timely access issues for these provider types. Both departments also noted that the most recent surveys occurred during the COVID‑19 pandemic, which may have affected the results. For example, Managed Health Care specifically expressed that several plans reported to the department that the low number of providers offering timely appointments was a result of staffing shortages and the accumulation of appointment demand related to the pandemic.
Although DHCS and Managed Health Care cited effects of the pandemic as possible reasons for low rates of compliance in their most recent surveys, neither department has collected and retained data allowing us to determine whether timely access for children is improving or getting worse. According to DHCS, the department did not survey plans for much of 2020 or any of 2021 because of the COVID‑19 pandemic. In addition, DHCS could only provide us with incomplete results of surveys of behavioral health care providers from before 2020. The data DHCS was able to provide from this period did not distinguish information regarding only children from the overall results for access to therapists, preventing us from comparing those results to the most recent survey.
Managed Health Care has explained that yearly changes in its survey methodology before 2019, such as clarifying the types of providers to be included and revising calculations of wait times to better align with the timely access standards, mean that survey results before 2019 are not comparable to the current results. Further, Managed Health Care does not measure appointment availability specifically for children. Managed Health Care was able to provide results for all appointments from 2019 to 2021, and a comparison of these results shows that timely access to therapists and psychiatrists did not improve over those years and, for some types of appointments, may have gotten slightly worse. Managed Health Care similarly reported in its timely access survey report for 2021 that the timely access rates for both urgent and non‑urgent appointments fell below the rates reported in the previous year. However, because of the lack of complete and comparable data over the past several years, we are unable to determine whether timely access for children specifically has improved or worsened.
Weaknesses in How DHCS and Managed Health Care Monitor Timely Access May Obscure the Full Extent of Access Issues
We identified several weaknesses in the methods the departments use to conduct their timely access surveys; these weaknesses could affect the usefulness of the survey results. Some stem from gaps in the departments’ measurement of urgent appointment types and of appointments specifically for children. Others may lead the published survey results to overstate the availability of timely appointments, particularly from the perspective of an actual patient or family.
A primary issue with the current survey results is that the survey methodologies exclude many of the providers DHCS and Managed Health Care attempt to survey. Surveyors use provider contact information supplied by the plans, and the surveyors exclude ineligible providers from the survey results if they learn, for example, that the providers do not provide the service being measured or no longer operate in a given service area, because those providers are therefore not relevant to the purpose of the survey. However, the survey methodology further excludes providers who simply do not answer the survey calls or who decline to participate in the survey. In the first half of 2022, roughly two‑thirds of the Medi‑Cal providers included in the DHCS survey were ultimately excluded from the calculation of the rate of appointments meeting timely access standards for these or other reasons. For its part, Managed Health Care’s data indicate that nearly 30 percent of therapists, for example, were deemed ineligible or non‑responsive in 2021. It would be reasonable to exclude providers who do not respond from those specific calculations. However, the resulting published conclusions about timely access may not be fully representative of each plans’ capacity to serve patients if the reports do not account for ineligible or non‑responsive providers by another means. For example, if providers without timely appointments are less likely to participate, their exclusion could risk overstating the availability of timely appointments across a plan.
Indeed, the departments’ survey results do not publicly report the number of or reasons for providers’ exclusion from the survey for each plan, affecting the results’ usefulness to members of the public. Managed Health Care’s website does include downloadable information on the raw number of providers excluded from each network surveyed, but members of the public would then need to analyze the data to reach their own conclusions. DHCS does not publish information on the responsiveness of providers beyond the total number of those excluded from the survey. As such, the results on timely access do not sufficiently account for significant barriers families may face when trying to obtain timely appointments. For example, in Molina Healthcare of California’s Medi‑Cal network, more than 70 percent of the therapists the surveyors attempted to reach were deemed ineligible or did not respond and therefore would be excluded from the corresponding rate of compliance calculations in Managed Health Care’s survey results. In scenarios like this one, a family seeking an appointment may call several providers before being able to contact one that is even offering relevant appointments. The departments’ surveys are designed to assess the timeliness of that last provider’s appointment, but the resulting reports do not provide enough information to make members aware of how long it may take them to reach that provider.
In practice, this gap in the survey’s published data diminishes the value and usefulness of the compliance thresholds; Managed Health Care sets its 70 percent compliance threshold based on its conclusion that in a plan achieving that threshold, nearly all members would be able to obtain a timely appointment in three or fewer calls. Actual plan members who experience frequent or repeated failed attempts to reach a provider therefore experience practical access limitations in ways the survey reports do not currently publish. For the same reason, the reports also may provide insufficient information for members who use the results when considering which plan to join. Both DHCS and Managed Health Care acknowledged that because of the number of ineligible and non‑responding providers to the survey, the surveys may not fully reflect members’ experiences. DHCS and Managed Health Care indicated to us that they are willing to explore ways to publish this information in conjunction with the timely access results to better inform stakeholders of these issues.
Plans’ inaccurate information about providers, which likely contributes to low survey response rates, is a related cause of access challenges for plan members seeking appointments. In a 2018 audit, our office found that DHCS’ method for reviewing provider information does not provide sufficient assurance of the accuracy of the provider data made available to members.Report 2018‑111, Department of Health Care Services: Millions of Children in Medi‑Cal Are Not Receiving Preventive Health Services, March 2019 We confirmed the persistence of this issue in a follow‑up report from 2022. Because DHCS had not done enough to ensure that its provider information was accurate, our September 2022 follow‑up audit concluded that DHCS potentially impeded families’ access to providers.Report 2022‑502, Follow‑Up: Children in Medi‑Cal: The Department of Health Care Services Is Still Not Doing Enough to Ensure That Children in Medi‑Cal Receive Preventative Health Services, September 2022 Until DHCS implements our related recommendation to improve the accuracy of public provider information, the reported information resulting from the surveys will not be as useful for members and their families as it should be.
There is also potential incentive for providers to give inaccurate information to the surveyors, because the individuals conducting the surveys announce who they are and the purpose of their call. Therefore, responding providers know that the caller is not a patient in need of an actual appointment and may simultaneously feel pressure to provide a response that aligns with the standards in law. By contrast, an article published in the Archives of Public Health journal in 2022 argues that surveyors’ masking their identity and posing as patients seeking care is a best practice for attaining a realistic and unbiased perspective of the patient experience. Both DHCS and Managed Health Care agreed that an approach wherein the surveyor posed as an individual seeking care (sometimes referred to as a “secret shopper” methodology) could be an improvement to the current method with regard to reducing the potential for provider bias, but expressed concerns with the practicality of that approach. For example, DHCS noted that providers need personal health coverage information before offering an appointment time, making such an approach more costly and complex. However, neither department has conducted a formal analysis of the feasibility of the approach to identify its likely costs and benefits. Because a proposed rule from CMS would require this “secret shopper” approach, which we also determined that at least one other state, Texas, currently uses, DHCS and Managed Health Care should study the costs and possible benefits of using such an approach to help ensure accurate and unbiased survey results.
Other issues with the surveys’ current methodologies create gaps in the departments’ abilities to measure timely access. For example, neither department currently monitors access under state law’s most stringent appointment wait time standard—urgent appointments for services that do not need prior authorization—for which patients should wait no longer than 48 hours. DHCS prohibits Medi‑Cal plans from requiring prior authorization for initial behavioral health assessment services or for crisis intervention provided by mental health plans, which means that the 48 hour standard would apply to such urgent appointments. Instead, both surveys measure these appointments against the 96 hour standard, which applies to urgent appointments for services that require prior authorization. Before our review, DHCS was not aware that its survey monitored all urgent appointments against the 96 hour standard and agreed that it is a limitation of the survey. After we made DHCS aware of the issue, it told us that it is working to update the survey methodology accordingly. Managed Health Care acknowledged that measuring compliance against the two separate standards based on the coverage requirements of specific plans would align with timely access standards, but it argued that doing so could result in more complex calculations for health plans and subsequent calculation errors. Managed Health Care also stated that because it would need to implement and refine the changes over time, it may delay any enforcement actions and need to recalibrate the 70 percent compliance threshold for these appointments. Although some ongoing refinement may be necessary, we believe that it is important for Managed Health Care to develop and implement an approach to replace its current practice of treating all urgent appointments the same. The fact that state law sets a specific standard for these urgent appointments that is half as long as the next‑shortest time frame clearly highlights the importance of monitoring access for the children who most need those services.
Another limitation in both departments’ surveys relates to appointments for new patients compared to existing patients. Neither DHCS’ nor Managed Health Care’s surveys capture the availability of timely appointments for both new and existing patients, even though availability with the same provider could differ. In both surveys, when a provider notes that the next available appointment would differ depending on whether the appointment was for an existing patient or a new one, the surveyor records and calculates the wait time for only the earlier appointment. Because of this approach, the appointment time recorded in the survey may not be representative of an actual patient’s experience when requesting an appointment. DHCS agreed that the survey is limited in the respect that it does not capture availability for new patients. Managed Health Care noted that, as part of required annual network reporting, health plans must identify whether each reported network provider is accepting new patients. Managed Health Care uses this information to measure the percentage of providers who are offering appointments for new patients in each plan’s network and at each reported provider location to determine whether there are sufficient numbers of providers to support timely access to care. However, the review does not actually assess the timeliness of appointments for new patients.
Finally, Managed Health Care’s survey does not measure appointment availability specifically for children, even though DHCS’ survey results indicate that the availability of timely access for children and adults can differ. As a result, Managed Health Care’s survey results may not accurately depict how available those appointments are for child patients. According to Managed Health Care, the department has not measured plans’ performance in meeting timely access standards for these different populations because there is no distinction in state law for timely access between children and adults. Managed Health Care agrees that there could be value in measuring appointment availability specifically for children, but it indicated that such an approach could significantly increase the sample size needed to produce reliable survey results and result in other administrative difficulties. According to Managed Health Care, this change could add to the State’s cost of administering the survey by requiring more employees to review the data for compliance and issue findings to health plans, which the department estimates would total roughly $700,000 per year, or about 0.4 percent of its 2023–24 budget. We acknowledge that this change in methodology may require increasing the sample size and therefore increasing the numbers of calls made or questions asked during a given call. Nevertheless, Managed Health Care and the public cannot effectively evaluate the extent to which children, specifically, have timely access to behavioral health care appointments using the existing approach.
In response to our findings regarding gaps in its survey methodology, Managed Health Care also expressed an interest in the possibility of replacing its survey approach with a method in which health plans would obtain historical patient appointment information from providers’ practice data management systems over the course of a year. Under such a method, providers would electronically provide actual patient appointment information necessary to measure compliance with existing timely access standards. Managed Health Care indicated that the feasibility of such an approach needs to be studied, including to determine the extent to which providers would need to update their data management systems in order to allow for the collection of appointment information in this manner. Although we did not analyze the benefits and costs of such an approach, to the extent Managed Health Care is able to demonstrate whether it is a viable option for improved measurement of timely access to care while also taking steps to ensure that it addresses the issues we identified, we encourage it to do so.
DHCS Should Take Further Action to Ensure That Children Are Receiving Specialty Behavioral Health Care From County Programs in a Timely Manner
Data on actual appointment times for specialty mental health services offered by counties show that those programs also struggle to meet timely access standards. Since 2018 state law has required county mental health plans to comply with timely access standards. In 2021 DHCS started requiring all county mental health plans to report data on appointment wait times for new plan members using a standardized format. Before fiscal year 2022–23, DHCS directed county mental health plans to meet a 70 percent compliance threshold for timely appointments offered. For fiscal year 2022–23, DHCS increased the compliance threshold to 80 percent to set what it characterized as a more rigorous standard.
Currently, a significant number of county mental health plans are not in compliance with DHCS’ timely access standards, and DHCS should do more to ensure that plans improve. In its fiscal year 2022–23 monitoring, DHCS identified 28 county mental health plans as noncompliant with timely access standards. DHCS requires county mental health plans not in compliance with timely access standards, including those who do not provide sufficient data to determine access, to submit a written plan demonstrating the steps the plan will take to achieve compliance. For example, San Bernardino County mental health plan provided to DHCS a list of action items it would accomplish to come into compliance, such as reminding its programs and contracted agencies of timely access standards. DHCS determined that the plan’s response was sufficient; however, according to the section chief, DHCS did not follow up with the plan to confirm that the county had actually implemented its plan because the narrative the plan provided demonstrated that it would be able to come into compliance.
DHCS’ records indicate that a significant number of county mental health plans remain out of compliance. DHCS required county mental health plans initially not in compliance with timely access standards to submit additional data on appointment wait times later in the year. However, after analyzing the additional information, DHCS determined that San Bernardino’s county mental health plan, along with 16 other county mental health plans—or more than a quarter of all such plans in the State—were still not demonstrating that they had met the 80 percent timely access compliance threshold. These counties are some of the largest in the State, including Los Angeles and Santa Clara counties. Although DHCS told us that very few plans would have been out of compliance under its previous 70 percent threshold, based on the current 80 percent standard, a significant number of members are currently being served by plans with insufficient timely access.
DHCS explained that the pandemic affected its efforts to perform further monitoring or enforcement of timely access for county mental health plans. According to the DHCS section chief, the department notifies county mental health plans of their continued non‑compliance status. The section chief also confirmed that DHCS did not impose any sanctions or conduct further investigation of these plans. The chief of the Oversight and Monitoring Division at DHCS (division chief) explained that DHCS did not take further enforcement actions against plans who continued to be out of compliance because of the COVID‑19 pandemic and the agency’s shift in focus to public safety and emergency operations, and she noted that DHCS has begun undertaking actions to develop clear criteria for the issuance of sanctions as part of its overall enforcement efforts and is working to communicate clearly with county plans about when and how sanctions will be deployed. The division chief further confirmed that starting in fiscal year 2023–24, DHCS is working on improvements to allow for more efficient reviews of county plans’ submissions and CAPs, and it also plans to conduct ongoing follow‑up with all plans that continue to be out of compliance after submitting a CAP, in addition to issuing financial sanctions in instances DHCS deems appropriate.
DHCS does not separately account for county mental health plans’ abilities to serve children when determining the plans’ compliance with timely access thresholds. According to the section chief, DHCS began collecting data specific to children in 2022. However, the department then combined all age groups when determining whether a county mental health plan meets the compliance threshold. This approach may obscure access issues for children within a given plan. For example, DHCS’ records indicate that Fresno County mental health plan satisfied the compliance threshold; however, the compliance percentage for children’s appointments was only 76 percent—more than 10 percent lower than the measured 88 percent compliance percentage for adults. In other words, the county would not have passed the compliance threshold if the children’s appointment availability had been evaluated separately. DHCS explained that it has measured compliance by looking at all appointments, regardless of age group, because the same timely access standards apply to both children and adults. However, DHCS’ assistant deputy director for behavioral health (deputy director) confirmed that because the fiscal year 2022–23 data showed a significant difference between adults’ and children’s appointment wait times for some county mental health plans, the department intends to begin measuring compliance for adults’ and children’s appointments separately starting in fiscal year 2023–24. If DHCS makes such an adjustment to its approach, it will be in a better position to address timely access issues specific to children in Medi‑Cal.
Although DHCS currently measures whether county mental health plans are meeting compliance thresholds for timely access, the department has not yet begun to measure compliance for all substance use services. Since 2022, state law has expressly required that appointments with substance use disorder providers comply with the same timely access standards as therapists. For fiscal year 2022–23, DHCS required Drug Medi‑Cal Organized Delivery System (DMC‑ODS) plans to submit timely access data along with county mental health plans. DHCS determined that of the 31 DMC‑ODS plans, 22 were in compliance with the 80 percent compliance threshold and nine were not. When establishing the reporting requirement, DHCS stated that it would not put any of the DMC‑ODS plans on CAPs if they were out of compliance for timely access. The section chief told us that the department did not do so because it was an advisory year for this monitoring, but he stated that DHCS did place plans on CAPs for other issues, including some we discuss later in the report. DHCS will require Drug Medi‑Cal Treatment Programs (DMC) to submit timely access data beginning in fiscal year 2023–24. The section chief confirmed that DHCS will follow the same process for monitoring DMC and DMC‑ODS plans as it intends to for county mental health plans.
Delays in Access Can Have Potentially Severe Consequences for Children
Our review of medical records and the results of our phone survey of behavioral health care providers indicate that there are significant risks for children who experience delays in accessing behavioral health services. In addition to the research showing that children who face these delays may be at an increased risk of adverse health effects of varying types and severity, we identified limited instances of these types of negative effects in our review of 54 patient medical records. A general lack of consistent, detailed information about appointment wait times in those records prevented us from linking documented negative outcomes specifically to access issues in most cases. Specifically, even when medical records indicated a negative health outcome, the records often lacked information that would be necessary to indicate a delay in access, such as when an appointment was requested. However, we did identify a case in which the worsening of a child’s condition was clearly tied to a delay in receiving behavioral health services. In this case, the medical record showed that a child’s parent requested an earlier appointment than their existing follow‑up appointment scheduled for two months later. The parent specifically requested that the appointment be outside of school hours. The provider scheduled an appointment for several weeks later and indicated that the patient should be added to a cancellation list. About a week after that request, the child’s parent called again and requested an urgent appointment out of concern about the child’s symptoms, but the record does not demonstrate that a sooner appointment was scheduled. Later the same day, the child was admitted to a hospital with suicidal and homicidal ideation. Although we were unable to reach a conclusion about whether this case indicates a violation of timely access standards, in part because the child’s parent requested an appointment only within certain hours, it does demonstrate the potentially harmful effects of delays in receiving behavioral health care.
In our survey of behavioral health care professionals who treat those enrolled in Medi‑Cal, providers reported similar effects from lack of timely access. We attempted to contact 144 providers and, of the 16 providers who responded, 13 described potential adverse effects for children in Medi‑Cal who experience delays in accessing behavioral health services. Four providers expressed concern that children who do not have timely access to behavioral health services could face a higher risk of suicide attempts or other self‑injury. Other providers noted that delays in receiving behavioral health services could lead to declines in academic performance or worsening of existing conditions. Specifically, two other medical records we reviewed contained assertions that prolonged or repeated periods without behavioral health services had resulted in escalating symptoms, such as increased tantrums or incidents of aggressive behavior.
Despite Compelling Evidence of Insufficient Provider Capacity for Children in Medi‑Cal, DHCS’ Monitoring Efforts Demonstrate Weaknesses
DHCS sets minimum provider‑to‑member ratios meant to help it determine whether plans will be able to meet the expected demand for services, but the ratios it sets require too few providers to achieve that result. In fact, managed care plans often had hundreds of times as many providers as the ratios require, despite the fact that many plans struggled to meet timely access standards. Although DHCS was unable to fully explain how it calculated the ratios, its methodology did include an overestimation of the amount of time providers spend treating children in Medi‑Cal and an over counting of providers who may contract with more than one plan or with the same plan in multiple regions. Further, DHCS approves standards for some Medi‑Cal plans that may require children in certain rural areas of the State to travel two hours or more for care. State law requires DHCS to consider the reasonability of such standards, but DHCS has not established a formal definition of reasonable times or distances to use for this purpose. Finally, DHCS has not used its CAP process, or its authority to impose sanctions, to sufficiently ensure that plans take meaningful steps to improve children’s access to behavioral health services.
Flaws in DHCS’ Provider Monitoring Undermine Its Efforts to Ensure Access
Contrary to evidence, including the significant timely access issues indicated by its own surveys, DHCS asserts both publicly and in its 2022 report to CMS that all Medi‑Cal plans have more than enough providers for their members who are children. A fundamental shortcoming in DHCS’ monitoring of provider capacity is DHCS’ focus on the total number of providers believed to be contracting with plans at a given point in time. As mentioned in the preceding section, our office has previously raised concerns about the accuracy of provider information available to Medi‑Cal members, and during this review we were unable to identify a sufficiently reliable data source for the total numbers of providers accepting Medi‑Cal in the State. Despite these issues, DHCS continues to simply count the providers in the plans’ electronic directory files when determining how many mental health providers plans have available to serve children. Our own analysis indicates that when assessing plans’ capacity to provide timely services to children, it is more relevant to consider the number of services a given provider delivers than to simply count the number of providers available to provide services to those enrolled in Medi‑Cal.
Our analysis of DHCS’ statewide data shows that the numbers of health care entities providing services to children in Medi‑Cal has not increased from 2017 through 2022, but that those entities are collectively providing more behavioral health services.Even though each behavioral health services claim may include multiple procedures provided by more than one individual, our analysis defined a health care entity as the provider reporting the claim to DHCS. The health care entity could be a single person or an organization. For consistency’s sake, we generally use provider to refer to both individuals and organizations except when discussing the results of this analysis. Specifically, as Table 2 shows, the total number of behavioral health services provided to children enrolled in Medi‑Cal increased by nearly 13 percent over this time period, while Medi‑Cal enrollment increased by only 2 percent. However, even with this increase in services overall, our analysis found that many health care entities providing behavioral health services, including psychologists, family therapists, and social workers, see those enrolled in Medi‑Cal only infrequently, as we discuss later. Despite the importance of how many services each provider delivers, DHCS’ current approach to monitoring plans’ capacity does not account for the number of providers actively treating patients or the extent to which they do so. To the extent barriers to access exist, so too does the potential for children to suffer the adverse effects of delays in or absence of behavioral health care. It is therefore important for DHCS to ensure that its monitoring efforts result in information that is sufficiently reliable for identifying provider shortages.
Table 2
The Number of Behavioral Health Services Increased Between 2017 and 2022
| Year | Number of Behavioral Health Services |
| 2017 | 11,835,374 |
| 2018 | 12,438,844 |
| 2019 | 13,046,043 |
| 2020 | 12,547,134 |
| 2021 | 13,788,805 |
| 2022 | 13,339,260 |
Source: DHCS claims data.
Examples of Quantitative Standards States May Use For Monitoring Medicaid Network Adequacy
- Minimum provider‑to‑enrollee ratios
- Maximum travel time or distance to providers
- Minimum percentage of providers that are accepting new patients
- Maximum wait times for an appointment
Source: CMS 2020 Final Rule.
As early as 2017, CMS reported that an overall shortage and uneven distribution of health care providers limit access to behavioral health services in public health care systems. Federal Medicaid regulations require that states develop quantitative network adequacy standards for specified types of adult and pediatric providers, including behavioral health care providers. The text box lists some examples of the quantitative standards that states may use. In California, DHCS sets minimum ratios of providers to members for various services to determine whether plans will be able to meet expected demand. DHCS requires both managed care plans and county mental health plans to meet provider‑to‑member ratios for various types of behavioral health care providers, including specialty and non‑specialty mental health providers. For example, in 2022 DHCS required county mental health plans to have one mental health provider for every 43 children requiring specialty mental health services within their county. However, we identified significant problems with the non‑specialty provider ratios that limit the ratios’ effectiveness as a monitoring and regulatory tool.
DHCS’ provider‑to‑member ratios for pediatric non‑specialty mental health care providers—psychologists, licensed family therapists, and licensed clinical social workers—do not provide meaningful assurance that plans will have sufficient numbers of providers to offer children timely access. Specifically, DHCS set the 2022 required provider‑to‑member ratio for these providers at only 1 provider per 116,000 child members. Based on data presented in a 2023 report from the CDC, this is an unreasonably low number of providers. The CDC report presented national survey data indicating that nearly 15 percent of children between 5 and 17 years old received some form of mental health services in 2021 and that more than 11 percent of children specifically received counseling or therapy from a mental health professional. Moreover, federal law relating to health workforce development programs generally designates a geographic region as having a shortage of mental health providers if, among other criteria, it has only one core mental health professional per 9,000 people. The federal definition of mental health professional includes provider types—psychiatrists and psychiatric nurse specialists—which DHCS does not include in its non‑specialty provider ratio and therefore limits the direct comparability of the two ratios. Nonetheless, given the fact that the federal ratio of a provider shortage—1:9,000—requires more than 10 times the number of providers as DHCS’ ratio of sufficient providers to members—1:116,000—it becomes clear that DHCS’ ratios are far too low to effectively measure whether plans have enough providers to meet the expected need for care.
In fact, if we applied DHCS’ 2022 ratio of one provider per 116,000 members to the State’s population of 5.7 million children in Medi‑Cal, it would result in a requirement that all managed care plans collectively have 49 full‑time pediatric non‑specialty mental health care providers in the entire State. However, the same year that DHCS established the minimum non‑specialty ratio of 1:116,000, it also established a ratio for county mental health plans of one specialty mental health provider for every 43 children that, when applied, required 9,700 full‑time pediatric specialty services providers throughout the State—or nearly 200 times as many providers than the non‑specialty ratio would have called for. Although specialty behavioral health services can be intensive, and therefore may require more providers per child needing those services, the disparity between the two ratios does not appear reasonable.
DHCS described the methodology it used to calculate the non‑specialty ratio, but when we asked about the specific numbers discussed above, DHCS did not explain why its work produced such low results. According to the chief of the Managed Care Networks and Access Branch (access branch chief) in DHCS’ Managed Care Quality and Monitoring Division, DHCS developed the non‑specialty ratio based on Medi‑Cal utilization of the three provider types discussed above for a specific set of mental health service categories—including psychiatric evaluation and various types of psychotherapy. If the data DHCS used accurately reflected the total use of behavioral health services by those providers, it would mean those three types of providers performed only about 55,000 Medi‑Cal services for children statewide in 2022, serving less than one‑tenth of one percent of enrolled children each month (even assuming just one service was provided for each of those children). By contrast, our own review of DHCS’ claims data found that in 2022 health care entities classified as psychologists, family therapists, and social workers reported 472,000 non‑specialty behavioral health services for children in Medi‑Cal—more than eight times DHCS’ estimate.Our analysis defined behavioral health services as Medi‑Cal claims in which behavioral health was the principal condition requiring medical attention. While each encounter can consist of multiple individual procedures that are collectively reported to DHCS on a claim, we counted each claim as one service. To align with DHCS’ method for calculating the non‑specialty ratio, we excluded fee‑for‑service claims and claims related to specialty mental health services and Drug Medi‑Cal programs from this calculation.
DHCS also did not fully explain the specific calculations that led to its determination of the low number of required providers. According to DHCS’ access branch chief, key data underlying DHCS’ calculations are unavailable because the sources used were temporary in nature and the staff members who performed the analysis are no longer at DHCS. Nevertheless, the federal standards relating to provider shortage areas, available research on behavioral health care demand, and the information in DHCS’ own claims data we used to analyze actual services provided all indicate that DHCS’ analysis is likely flawed.
DHCS Determined That Five Plans Had More Than 1,000 Times As Many Providers as Required in 2022
| Plan | Number of Providers DHCS Required | Number of Providers DHCS Identified | Number of Times as Many as Required |
| Aetna Better Health of California | 0.23 | 509 | 2,213 |
| Kaiser | 1.25 | 1,483 | 1,186 |
| Partnership HealthPlan of California | 3.61 | 4,649 | 1,288 |
| San Francisco Health Plan | 0.67 | 970 | 1,448 |
| Santa Clara Family Health Plan | 0.41 | 992 | 2,420 |
Source: DHCS Non‑Specialty Mental Health Provider Ratios for 2022.
Note: Numbers of providers shown are total for all regions served by each plan.
DHCS had other reasons to question the results of its analysis of the required number of non‑specialty mental health care providers. DHCS’ low provider‑to‑member ratios would indicate that every Medi‑Cal managed care plan in the State had far more providers available than the minimum required. In fact, when we applied the ratio DHCS used to calculate the supply of providers in 2022, the results said that every managed care plan had at least 80 times as many pediatric non‑specialty providers as DHCS required. As the text box shows, five of the 24 plans had more than 1,000 times as many providers as required. However, the department’s other monitoring activities concluded that many of the plans struggled to offer children in Medi‑Cal timely mental health appointments. Figure 7 provides an example of a plan that far exceeded the minimum non‑specialty provider ratio in one county but still struggled to ensure timely access that year. By way of comparison, DHCS found that just 30 of the 57 county mental health plans met the required pediatric specialty services ratio in 2022, and only 33 met the related pediatric psychiatry ratio. The county plan results better reflect the difficulties the plans faced in providing timely appointments.
Figure 7
An Example of a Plan for Which DHCS’ Provider‑to‑Member Ratios for Plans Did Not Correlate With the Plan’s Ability to Provide Timely Access
Source: DHCS provider ratio data, 2022 Medi‑Cal Timely Access Survey Data, state law.
Figure 7 description:
This figure consists of 2 different bar charts. The first one depicts the number of providers Central California Alliance for Health plan was required by DHCS to have in one county versus the number of actual providers the plan had. The bar chart is labeled "Number of Providers." The bar chart shows one bar, labeled "required", showing the result of 1. The second bar, labeled "actual", shows the result of 23. To the right, there is text that reads "DHCS determined that the Central California Alliance for Health plan had 23 times the number of outpatient behavioral health care providers in one county as required." The second bar chart is below and is labeled "Percentage of Appointments Meeting Timely Access Standards." The first bar is labeled "non-urgent" and shows the result of 24.4%. The second bar is labeled "urgent" and shows the result of 65.3%. To the right, there is text that reads "However, the plan was frequently unable to offer timely appointments in accordance with state law."
Despite DHCS’ inability to fully explain how it calculated the minimum non‑specialty mental health provider ratios, we identified two key flaws in its approach to determining whether plans had enough providers to meet members’ needs. The first flaw results in DHCS’ overestimation of how many hours each month non‑specialty providers spend treating children in Medi‑Cal. To calculate how many providers each plan needs, DHCS assumes that each provider will spend 96 hours per month (about 24 hours per week) treating Medi‑Cal patients. DHCS based this number on feedback from stakeholders indicating that behavioral health care providers spend, on average, 60 percent of their time providing services directly to patients, and they spend the remaining 40 percent of their time on administrative‑type activities. However, it is highly unlikely that every provider in a plan will spend all of their treatment time seeing only Medi‑Cal patients. In fact, when we analyzed DHCS’ behavioral health services data, we found that of the 3,500 health care entities classified as psychologists, family therapists, and social workers we identified as reporting providing behavioral health services to children in Medi‑Cal in 2022, nearly half of them provided fewer than two services per month to children in Medi‑Cal.
In a specific example relevant to the ratios’ effects on timely access, our analysis determined that in 2022, the plan depicted in Figure 7 had 23 different psychologists, family therapists, and social workers provide the types of services DHCS considered when developing its ratios to children enrolled in Medi‑Cal, equivalent to the reported number of 23. However, nearly half of the providers delivered fewer than 10 of these Medi‑Cal services for the plan over the entire year, or less than one per month on average.
Therefore, when counting how many providers plans have, DHCS should count the providers based on the portion of their time they actually spend treating Medi‑Cal members. In other words, if a plan’s provider spends half of their time treating Medi‑Cal patients, and the other half of the time treating patients outside of Medi‑Cal, DHCS should credit that plan with half of a provider when determining whether the plan complies with the required non‑specialty provider ratios. DHCS already requires county mental health plans to count their providers in this way, but it does not require managed care plans to do so. The access branch chief indicated that DHCS is researching whether it can conduct a similar analysis for managed care plans using the provider data DHCS currently has. Whether with that data or by another means, DHCS should better account for the amount of time providers spend treating Medi‑Cal members. Otherwise it will continue to misrepresent the capacity of plans’ providers to deliver services to Medi‑Cal members.
A second, related flaw in DHCS’ calculation is that it counts non‑specialty mental health providers more than once if they contract with multiple plans or with the same plan in multiple regions. For example, in 2022 DHCS determined that Partnership HealthPlan of California, which operates as the sole Medi‑Cal managed care plan in 14 Northern California counties, had a total of 4,649 pediatric non‑specialty mental health care providers. Of these, DHCS counted exactly 714 providers in each of two of the four regions covered by the plan, and 1,610 and 1,611 providers in the other two regions, respectively. The access branch chief confirmed that the same provider can serve multiple regions, and it would be reasonable to assume that there is a high overlap of providers in these sets of regions. To the extent that is true, it means that DHCS—at a minimum—double‑counts the availability of these providers to serve Medi‑Cal members. We saw multiple such occurrences of possible overlap in DHCS’ provider analysis. According to DHCS, it already takes steps to help account for this issue when it calculates ratios for other types of providers. For example, the access branch chief described a process for calculating physician provider‑to‑member ratios in which DHCS divides a provider’s expected contribution to a plan across the different counties and sites the provider serves. However, DHCS does not currently account for such factors when it calculates the non‑specialty mental health provider ratios. Figure 8 illustrates a hypothetical example of a behavioral health provider who spends half of their time with Medi‑Cal members within a plan that serves three separate regions. If that provider appears in the plan’s provider directories for each of those regions, then DHCS’ conclusion that the single provider represents three full‑time Medi‑Cal providers would overstate that provider’s actual contribution to the plan’s capacity as six times the actual contribution.
Figure 8
The More Regions a Provider Serves, the More DHCS’ Approach Overestimates the Plan’s Capacity to Serve Its Members
Source: DHCS’ described methodology for calculating non-specialty outpatient behavioral health care provider-to-member ratios for Medi-Cal Managed Care Plans.
Figure 8 description:
This figure shows a bar chart consisting of three bars representing a number of regions from one region to three regions. The bottom of each bar is blue and the top is dark orange. The legend indicates that the blue portion of a bar is "a provider's contribution to a plan's capacity." A legend indicates the dark orange top portion is DHCS’ calculation of a provider's contribution to a plan's capacity." The first bar is labeled below the axis as "If the provider serves members from one region only," the second bar is labeled "If the provider serves members from two regions," and the third bar is labeled "If the provider serves members from two regions." The first bar shows the blue color at 50 percent, the dark orange at 100 percent, and red text above the bar saying “2X”. The legend indicates that the red text is "the resulting overestimation of a hypothetical provider's contribution of a hypothetical provider's contribution to a plan's capacity". The second bar shows the blue color also at 50%, the brown color at 200%, and the red text above it reads "4x." The third bar shows the blue color still at 50%, the brown color at 300%, and the red text above it reads "6x."
In addition to not reliably determining how many non‑specialty providers a plan needs, DHCS’ monitoring does not account for how many distinct providers a plan may actually have. This overlap between regions within a plan is likely reasonable in practice and could provide Medi‑Cal members with more provider options overall. In fact, we also noted that some Medi‑Cal providers report serving multiple distinct plans. However, DHCS should better account for the overlap’s effects on the number of providers needed for each plan, such as by reducing the expected contribution of a provider to a given plan when that provider serves multiple plans or regions within a plan. According to the access branch chief, DHCS will explore considering additional factors when determining non‑specialty provider ratios in the coming year.
Providers and plans we surveyed offered perspective that was consistent with our analyses. During our review, behavioral health care providers and officials at Medi‑Cal managed care plans expressed concerns that shortages of Medi‑Cal providers may affect access to behavioral health services. Officials of all four Medi‑Cal plans we spoke to cited a lack of Medi‑Cal providers as a barrier to children’s ability to access behavioral health services. Additionally, of the 16 providers we spoke to, nearly half expressed concerns related to providers’ willingness or ability to see members enrolled in Medi‑Cal. Three providers explained that they were currently not treating Medi‑Cal patients or were transitioning away from doing so; all three cited low Medi‑Cal compensation rates as a key factor. Four other providers that were treating Medi‑Cal patients offered perspective that low compensation rates were a barrier preventing them or others from serving a higher number of Medi‑Cal patients.
Collectively, the flaws in DHCS’ methodology for setting and determining plans’ compliance with provider‑to‑member ratios for non‑specialty mental health providers negate a key benefit those ratios could serve—to detect the need for additional behavioral health care providers in specific areas of the State and to drive subsequent action necessary to increase provider numbers.
Despite Having Made Progress, DHCS Still Approves Some Standards Requiring Members to Travel Unreasonable Distances to Access Care
The State’s Primary Time or Distance Standards for Behavioral Health Care Providers
Psychiatry Care and Outpatient Mental Health Services (adult and pediatric)
- Dense Counties: 30 minutes or 15 miles
Alameda, Contra Costa, Los Angeles, Orange, Sacramento, San Diego, San Francisco, San Mateo, Santa Clara - Medium Counties: 60 minutes or 30 miles
Marin, Placer, Riverside, San Joaquin, Santa Cruz, Solano, Sonoma, Stanislaus, Ventura - Small Counties: 75 minutes or 45 miles
Amador, Butte, El Dorado, Fresno, Kern, Kings, Lake, Madera, Merced, Monterey, Napa, Nevada, San Bernardino, San Luis Obispo, Santa Barbara, Sutter, Tulare, Yolo, Yuba - Rural Counties: 90 minutes or 60 miles
Alpine, Calaveras, Colusa, Del Norte, Glenn, Humboldt, Imperial, Inyo, Lassen, Mariposa, Mendocino, Modoc, Mono, Plumas, San Benito, Shasta, Sierra, Siskiyou, Tehama, Trinity, Tuolumne
Source: State Law and DHCS.
State law requires Medi‑Cal plans to meet standards for the maximum time or distance a member must travel for care for a variety of different types of behavioral health care providers, including psychiatrists and outpatient behavioral health care providers. These standards are designed to ensure reasonable access to that care, and the law requires plans to demonstrate compliance with these standards separately for adult and pediatric services for each provider type. DHCS assesses plans’ compliance with the standards for each ZIP code in the plans’ service areas. For psychiatrists and outpatient mental health care providers, such as therapists, the standard varies by county across four categories, as the text box shows. When plans cannot meet the time or distance standards, state law requires them to submit to DHCS a request for alternative access standards. DHCS must approve or deny the requests on a ZIP code and provider‑type basis, and it may approve those requests if the plan has exhausted all other reasonable options to obtain providers to meet the applicable standard. When DHCS is evaluating the request, the law also requires the department to determine whether the time or distance resulting from the request is reasonable to expect members to travel to receive care. The law requires DHCS to evaluate these requests, and DHCS conducts its review by considering factors such as whether the plan has attempted to contract with new, closer providers, or has explained why it did not do so.
In accordance with state law, DHCS also allows plans that meet certain requirements to offer members clinically appropriate telehealth appointments in lieu of requesting an alternative access standard. However, DHCS requires plans to offer affected members in‑person appointments if the member prefers, and it requires plans to provide members with transportation to those appointments.
There are fewer alternative time and distance standards in place now for plans than several years ago, but DHCS still approves some standards for non‑specialty mental health providers (therapists) and psychiatrists that may require children in Medi‑Cal in certain locations to travel significant distances to see behavioral health care providers. CMS states that timely access to high‑quality services in an equitable and consistent manner is key to the effectiveness of the Medicaid program. When we reviewed DHCS’ oversight of these standards in 2019, we found that the department had approved nearly 10,000 requests for alternative access standards.Report 2018‑111, Department of Health Care Services: Millions of Children in Medi‑Cal Are Not Receiving Preventive Health Services, March 2019 DHCS’ data indicate that by 2022, the number of alternative access standards it had approved statewide had declined by almost half to 5,500. According to the access branch chief, much of the reduction was due to correcting administrative errors, such as resolving duplicative requests that plans submitted. The access branch chief further asserted that DHCS’ efforts to hold plans accountable for attempting to contract with closer providers and plans’ building relationships with providers in the process also played a role in the reduction. Finally, the access branch chief explained that plans’ increased use of telehealth has also contributed to the reduction in the number of requests for alternative access standards plans submitted.
However, DHCS is still unable to demonstrate that it has done all it can to ensure that all of the current alternative standards contain reasonable travel times and distances. Indeed, DHCS has not formally defined how it determines that times and distances are reasonable. The access branch chief asserted that the requests for alternative access standards go through several levels of internal review before they are approved. Although DHCS may conduct multiple levels of review, it has not yet established a formal definition of reasonable times or distances to use when assessing a requested standard’s reasonableness during that process. The access branch chief agreed that DHCS could work to establish criteria for reasonable time and distance to consider as one part of the review process. Nevertheless, DHCS’ current alternative standards sometimes force Medi‑Cal members to travel significant and unequal times or distances to access behavioral health care.
Specifically, in 2022 DHCS approved more than 150 alternative access standards for pediatric psychiatrists and therapists providing non‑specialty mental health services. Forty of those alternative standards could require children to travel two hours or more to receive care. Table 3 shows a selection of the most extreme examples for these provider types. Although these are only a small portion of all alternative standards, and correspond to remote and rural areas of the State, DHCS nevertheless should do all it can to ensure that all children in Medi‑Cal have access to care within reasonable travel times and distances.
Table 3
In Some Rural ZIP Codes in Certain Counties, Children May Have to Travel for More Than Two Hours to See a Behavioral Health Care Provider
| Psychiatrists | ||
| County | Max Approved Driving Minutes | Max Approved Driving Miles |
| San Bernardino* | 215 | 190 |
| Inyo | 205 | 200 |
| San Diego | 150 | 130 |
| Riverside | 135 | 130 |
| Therapists | ||
| County | Max Approved Driving Minutes | Max Approved Driving Miles |
| San Bernardino* | 195 | 145 |
| Riverside | 125 | 130 |
Source: DHCS 2021–2022 Annual Network Certification, letter to a plan, and list of alternative standards DHCS approved.
* The maximum approved time and distance in this county are from different ZIP codes.
Further, DHCS has approved alternative access standards that create inconsistent times and distances in some areas. As an example, for two plans serving San Bernardino County, DHCS approved alternative access standards for pediatric psychiatry for different areas within the county, but the approved times and distances were not always consistent within each ZIP code. In one particularly notable example involving members living in one rural ZIP code in the county, DHCS approved an alternative access standard for psychiatrists of 110 minutes and 85 miles for one plan and an alternative standard of 210 minutes and 170 miles for the other. In so doing, DHCS deemed it reasonable that members of one plan may have to travel twice as far as members of another plan living in the same area. Table 4 lists other examples of alternative access standards DHCS approved for different plans with inconsistent times and distances within the same ZIP code. According to the access branch chief, these inconsistencies can arise when providers decline to contract with multiple Medi‑Cal plans. The access branch chief also stated that DHCS finds the discrepancies in access disconcerting and indicated that DHCS makes an effort to close provider gaps by sharing information with groups seeking to increase provider participation through rate increases and student loan repayment programs. However, the access branch chief confirmed that DHCS does not require plans to expand their own recruitment efforts beyond showing evidence of attempts to contract with closer providers.
Table 4
Some of DHCS’ Approved Alternative Access Standards for Time or Distance to Pediatric Behavioral Health Care Providers Are Inconsistent and Create Potential Disparities
| Managed Care Plan |
County | ZIP Code | Pediatric Provider Type | Standard | Minutes by Car | Miles |
| Molina Healthcare of California | San Bernardino | 92332 | Psychiatry | 75 minutes/ 45 miles |
215 | 185 |
| Inland Empire Health Plan | 135 | 130 | ||||
| Molina Healthcare of California | 92309 | 210 | 170 | |||
| Inland Empire Health Plan | 110 | 85 | ||||
| Molina Healthcare of California | 92364 | 185 | 185 | |||
| Inland Empire Health Plan | 150 | 135 | ||||
| Molina Healthcare of California | 92364 | Therapists | 130 | 120 | ||
| Inland Empire Health Plan | 100 | 85 | ||||
| Aetna Better Health | San Diego | 92004 | Psychiatry | 30 minutes/ 15 miles |
150 | 130 |
| Molina Healthcare of California | 95 | 70 | ||||
| Community Health Group | 92086 | 135 | 75 | |||
| United Healthcare | 70 | 55 | ||||
| Community Health Group | 92004 | Therapists | 100 | 95 | ||
| United Healthcare | 65 | 60 | ||||
| United Healthcare | 91906 | 75 | 50 | |||
| Aetna Better Health | 35 | 35 |
Source: DHCS’ 2021–22 Annual Network Certification, DHCS’ alternative access standard request determination letter to a plan, and a list of alternative access standards DHCS approved.
DHCS also confirmed that it does not currently have a means of demonstrating how frequently its oversight of compliance with time and distance standards resulted in plans making improvements, such as identifying and contracting with new providers to reduce travel times. According to the access branch chief, the reasons why DHCS may deny a plan’s alternative access standards request include if DHCS locates a closer out‑of‑network provider than the plan identified in its request or if DHCS deems the plan’s justification for its inability to contract with a closer out‑of‑network provider to be insufficient. In such scenarios, the plan must revise its request accordingly and resubmit. However, the access branch chief separately indicated that even when DHCS identifies additional providers, the timing of the process means that new contracts are not usually in effect until the following year. Notwithstanding any delays in the availability of measurable results for the most recent year of 2022, DHCS could not provide summary‑level records of how many alternative access requests it initially rejected through its iterative process, nor can it track how many times its intervention resulted in plans’ contracting with closer providers, thereby reducing the time or distance of the alternative access standard DHCS ultimately approved. Instead, the access branch chief indicated that one could only determine those results from individually reviewing every plan’s request and approval.
Although state law requires Medi‑Cal managed care plans to maintain a network of providers that meets the time and distance standards discussed above, that law does not grant DHCS or the plans the authority to compel providers to contract with a plan in order to meet those standards. Nonetheless, DHCS could do more to help provide members with reasonably close and consistent access in instances where such contracting efforts have not been successful. According to the access branch chief, DHCS does not require plans to attempt to recruit new providers to areas where there are no closer providers. Further, as we describe previously, DHCS has not formally defined what times and distances are reasonable or identified criteria with which to make that determination, apart from conducting the review process described in this section. Finally, although DHCS’ policy is to require plans on a CAP to allow their members to see out‑of‑network providers, as we describe further in the next section, DHCS no longer required plans to do so once it closed the CAPs we reviewed. From 2021 through 2022, only a small number of plans were subject to the out‑of‑network requirement of DHCS’ CAP process. Employing such an approach more broadly could help reduce disparities in access for children in different plans. If DHCS established criteria defining reasonable travel times and distances for members, it could hold plans accountable by rejecting unreasonable alternative standards requests and requiring plans to remain on CAPs until they can ensure reasonable travel times and distances for their members.
DHCS’ Oversight Activities Do Not Sufficiently Address Barriers to Access
In the relatively rare instances when plans that do not meet time or distance standards in state law also do not have alternative standards approved, DHCS will place the plan on a CAP. DHCS requires plans to report on their progress every month until they have corrected the underlying deficiencies. DHCS informs plans that they have six months to correct the deficiencies identified in the CAP, and it has authority to impose financial sanctions on plans that do not comply with the terms of the CAP.
However, DHCS cannot demonstrate that its enforcement of recent CAPs has meaningfully improved access to care. In November 2021, DHCS placed five Medi‑Cal managed care plans on CAPs for deficiencies related to the time or distance standards: two of the CAPs applied to pediatric mental health providers. DHCS’ records indicate that these CAPs typically only resulted in plans submitting missing or corrected documentation, and none of the five plans demonstrated to DHCS that they had added providers to better meet time or distance standards. For an example of one of the CAPs, DHCS placed Aetna Better Health on such a plan in November 2021, because of its failure to comply with time or distance standards for a range of provider types in two counties, including therapists and psychiatrists in San Diego County. However, DHCS closed the CAP in April 2022, reporting that Aetna had submitted data demonstrating where its providers were and requested alternative access standards for provider types for which it did not meet the standards. DHCS also placed Anthem Blue Cross on a CAP after it failed to comply with time or distance standards in five counties, including for therapists and psychiatrists in Butte County. Again, DHCS closed the CAP after Anthem submitted updated data about the locations of providers and again requested alternative access standards.
In an example of a CAP that did not involve pediatric mental health providers but is emblematic of the process’s limitations, DHCS placed Molina Healthcare on a CAP but then closed it after Molina reported efforts to add new providers. However, DHCS’ evaluation of the plan’s efforts made no mention of whether the plan actually increased its provider numbers or improved availability to members. Instead, DHCS collected documentation from the plan describing that it had mailed letters of interest to the nearest providers. DHCS also does not, for example, require plans to attempt to recruit providers to relocate to underserved areas, such as by offering financial incentives. The access branch chief said that imposing such a requirement would be difficult. When we followed up to ask why, the access branch chief responded that, according to federal rules, plans can only use a certain portion of funding they receive for serving Medi‑Cal members on activities that are not defined as delivering medical services. According to the access branch chief, incentivizing providers to come into a plan’s network would not be considered delivering medical services. However, DHCS may still have options for requiring more evidence of plans’ undertaking new and creative efforts to address provider shortages, such as advertising in medical journals or conducting other forms of outreach.
DHCS includes provisions in CAPs that are intended to increase member access during the period over which the CAP is in effect, but those efforts may not meaningfully increase access to care. When DHCS placed these managed care plans on CAPs because the plans were not able to meet time or distance standards, it also imposed a temporary requirement that the plans authorize members to receive out‑of‑network access to providers who are not part of the plan. When it does so, DHCS also informs the plan that failure to comply with this provision of the CAP will result in financial sanctions. We reviewed documentation of DHCS’ efforts to enforce the out‑of‑network provisions for two plans on CAPs—the Inland Empire Health Plan and Molina Healthcare. To enforce the terms of the CAPs, DHCS directed the plans to submit call center scripts and training materials to ensure that staff were aware of the out‑of‑network requirement. DHCS also conducted telephone surveys with both plans to enforce compliance with the requirement.
In January 2022, DHCS notified the plans that it had conducted 10 calls to each and found them both to be out of compliance with the CAP requirement related to authorizing out‑of‑network access. The following month, DHCS reported conducting another 10 calls to each plan with the same result. According to the letters DHCS sent to each plan, during the second call campaign member services staff continued to provide responses based on the plan’s standard process rather than the process mandated by the CAP to inform members about their temporary access to out‑of‑network care. DHCS advised each plan to work with its staff and warned of potential financial sanctions if they continued to be non‑compliant. In March 2022, DHCS informed the plans that it had conducted a third round of calls and had found that both plans were compliant with the temporary requirements for allowing out‑of‑network access. However, the considerable enforcement efforts DHCS made in these two cases had no sustained effect on members’ access to care.
Within three weeks of the plans achieving compliance, DHCS closed both plans’ CAPs and eliminated the requirement that they authorize out‑of‑network access because those plans had provided the necessary documentation for DHCS to approve alternative time and distance standards. Given this sequence of events, it is doubtful that many of the plans’ members benefited from improved access to care during the time the requirements of the CAPs were in effect. And once again, neither plan demonstrated contracting with additional providers as part of completing its CAP.
Given the apparent limitations of CAPs to affect lasting change, DHCS could do more to improve access for members by focusing additional efforts outside of the CAP process. For example, during the period of our review, DHCS did not require plans to authorize out‑of‑network care unless the plan was on a CAP—even if those plans could not meet the time and distance standards in state law. Given that one component of DHCS’ review of plans’ requests for alternative time and distance standards is the requirement that plans attempt to add providers to their network, DHCS could increase the positive impact of its review by identifying and rejecting unreasonable alternative access requests from plans and thereby require those plans to pay for services that are available locally to members—even if the providers in question are not part of the plans’ networks. According to the access branch chief, as part of its annual process improvement activities, DHCS is considering changing its policy to include such a requirement. Although such a change would not address situations in which there is simply no closer provider, it could better ensure that children in Medi‑Cal generally have access to nearby providers and help reduce disparities in access to care.
DHCS also has not used its authority to impose financial sanctions on plans that fail to meet the network adequacy requirements. According to DHCS, plans may face sanctions if they fail to provide necessary documentation or provide inaccurate information, if they continually fail the out‑of‑network validation process, or if they fail to address all deficiencies within the CAP’s six‑month time frame. Although there is evidence of plans’ noncompliance with these requirements as recently as 2022, the access branch chief was not aware of any instance in which DHCS had imposed sanctions in response. For example, DHCS placed Anthem on a CAP in November 2021 but did not close the CAP until almost 11 months later in late September 2022. According to the access branch chief, Anthem continued to have administrative issues with its submission, and the CAP took longer than six months to close. The access branch chief said that during this time, DHCS continued to require Anthem to be subject to the CAP’s provisions, including monthly reporting and providing members with out‑of‑network access. The access branch chief said that DHCS made clear the expectation that such delays would open the plan up to further enforcement action in following years, but it did not issue any monetary sanctions. The access branch chief explained that DHCS refrained from imposing sanctions because of the COVID‑19 pandemic, believing that such sanctions were not appropriate given the extraordinary pressures plans were under, and it was important that managed care plans focused their resources on maximizing care delivery during that time. In August 2022, DHCS issued a letter to managed care plans clarifying its policy for imposing sanctions on plans, and that letter references DHCS’ legal authority to impose sanction on plans that fail to comply with network adequacy standards and CAP requirements. Although financial penalties alone are unlikely to resolve access challenges, DHCS’ consistent use of its authority when warranted could provide plans with appropriate incentives to comply with DHCS’ requirements.
DHCS also imposes CAPs on county mental health plans that fail to meet standards related to timely access and network adequacy, including time and distance standards and provider‑to‑member ratios. DHCS’ records indicate that, in addition to the 28 county mental health plans that DHCS placed on a CAP in fiscal year 2022–23 for being out of compliance with timely access standards, DHCS placed another 21 of the 57 county mental health plans on CAPs for being out of compliance with other network adequacy standards. Further, DHCS placed 25 of the county DMC‑ODS plans on CAPs for being out of compliance with network adequacy standards, including time or distance standards. However, as we describe previously, after DHCS placed these county plans on CAPs, it typically did not follow up to determine whether the plans had implemented all the corrective actions they proposed, nor did DHCS take any additional enforcement action for plans that remained out of compliance later in the year. At the end of fiscal year 2022–23, a total of 23 county mental health plans remained out of compliance with network adequacy standards, including time and distance standards and the timely access standards discussed earlier in the report, and 12 of the DMC‑ODS plans remained out of compliance. The section chief stated that starting in January 2024, DHCS will consider imposing sanctions, which could include financial sanctions, on county plans that do not come into compliance after DHCS places them on a CAP. Until DHCS conducts additional review and, when warranted, takes additional enforcement actions, there is little to encourage county plans to come into compliance and improve children’s access to these behavioral health services.
Recommendations
Department of Health Care Services and Department of Managed Health Care
To better ensure appropriate and effective monitoring of timely access to behavioral health care for children, by November 2024 DHCS and Managed Health Care should make changes to their survey methodologies to do the following, and then implement those changes for the subsequent reporting period:
- Use their timely access surveys to monitor compliance with the 48 hour urgent appointment standard established in state law where applicable.
- Disclose the proportion of providers excluded from their survey results for each plan, the reasons for excluding those providers, and how such exclusions may affect the survey’s conclusions about access to care.
- Use their timely access surveys to monitor compliance with the timely appointment standards for both new and existing patients.
To assess opportunities to help ensure unbiased timely access survey data, by November 2024, DHCS and Managed Health Care should determine the feasibility, costs, and likely benefits of adopting a “secret shopper” approach to their timely access surveys. If the departments determine that adopting such an approach is reasonably feasible and beneficial, they should implement this methodology by the next reporting year.
Department of Health Care Services
To improve its ability to use timely access surveys as a tool to improve access to behavioral health services, by November 2024, DHCS should develop a compliance threshold for the percentage of appointments in each Medi‑Cal managed care plan meeting timely access standards. For example, DHCS might consider how many calls a member should have to make before obtaining a timely appointment and calculate a threshold accordingly.
To help determine whether timely access to mental health services for children is improving, by November 2024, DHCS should report in each year’s timely access survey results on the extent to which those results are comparable to previous years’ results and, where data is comparable, discuss the extent to which timely access to care is improving or declining.
To improve Medi‑Cal members’ access to behavioral health services from county mental health plans and Drug Medi‑Cal programs, by November 2024, DHCS should demonstrate that it has followed up with county mental health plans and Drug Medi‑Cal programs on CAPs that continue to be deficient in timely access or other network adequacy standards. In doing so, it should assess whether the plans took the actions described in their CAPs and, if so, why those actions did not result in sufficient improvement.
To ensure that Medi‑Cal managed care plans have a sufficient number of providers to offer timely access and meet children’s behavioral health care needs, by May 2024, DHCS should develop a new methodology for calculating non‑specialty outpatient behavioral health provider‑to‑member ratios. At minimum, the methodology should consider the following factors:
- The expected demand for behavioral health services by children in Medi‑Cal, based on factors including but not limited to past services.
- The estimated number of children likely to need those services.
- The number of full‑time providers needed to provide that volume of services.
- The amount of time individual providers spend treating Medi‑Cal members.
The methodology should also accommodate potential growth in the need for behavioral health services.
To ensure that Medi‑Cal managed care plan members do not have to travel unreasonable times or distances to receive care, DHCS should develop a definition of what times and distances are reasonable for members to travel. In doing so, DHCS should consider both the total time or distance a member needs to travel, as well as how those times and distances compare to other plans’ times and distances for the same provider type and ZIP code. Thereafter, when DHCS determines that plans’ requests for alternative time and distance standards are not reasonable, it should not approve those alternative access standards, thereby requiring those plans to offer members out‑of‑network access until such time as the plans can provide reasonable travel times and distances to care.
To ensure that Medi‑Cal managed care plans make efforts to obtain additional providers to meet network adequacy standards, by May 2024, DHCS should revise its agreements with plans that do not meet time and distance standards to require them to demonstrate efforts to recruit new providers to underserved areas.
Department of Managed Health Care
To identify and address timely access issues that affect children, by November 2024, Managed Health Care should update its survey methodology to assess compliance with timely access standards specifically for behavioral health care providers serving children.
We conducted this performance audit in accordance with generally accepted government auditing standards and under the authority vested in the California State Auditor by Government Code section 8543 et seq. Those standards require that we plan and perform the audit to obtain sufficient, appropriate evidence to provide a reasonable basis for our findings and conclusions based on the audit objectives. We believe that the evidence obtained provides a reasonable basis for our findings and conclusions based on our audit objectives.
Respectfully submitted,
GRANT PARKS
California State Auditor
November 28, 2023
Staff:
Mark Reinardy, Audit Principal
Joshua Hooper, CIA, CFE
David F. DeNuzzo, CIA, CFE
Kate Monahan
Sunny Yan
Data Analytics:
Ryan P. Coe, MBA, CISA
Grant Volk, MA, CFE
Legal Counsel:
Natalie Moore, Senior Staff Counsel
Appendices
Appendix A—DHCS’ 2022 Timely Access Survey Results for Children
Appendix B—Behavioral Health Services Delivered Per Beneficiary in 2022
Appendix C—Children’s Emergency Department Visits for Behavioral Health Care
Appendix D—Scope and Methodology
Appendix A
DHCS’ 2022 Timely Access Survey Results for Children
In 2022, DHCS conducted a timely access survey for 24 Medi‑Cal managed care plans. Figure A on the following page shows the rates at which each of the plans met the timely access standards against which DHCS measures for urgent and non‑urgent appointments. An excerpt of this data appears as Figure 4.
Figure A
DHCS 2022 Timely Access Survey Results for Children, by Plan
Source: DHCS’ 2022 Medi‑Cal Timely Access Survey Data and Medi‑Cal Managed Care External Quality Review Technical Report.
Note: The percentage presented for each plan is the percentage of non‑urgent and urgent appointments available within timely access standards during DHCS’ timely access survey. The percentages only include the survey results for therapists and are measured against a standard of 10 business days for non‑urgent appointments and 96 hours for urgent appointments. As we discuss, DHCS’ use of the 96 hour urgent appointment standard for all therapist appointments is incorrect. Enrollment totals as of June 2022.
To view a larger version of Figure A, please click on the above image.
Figure A description:
This figure contains the results of DHCS' 2022 timely access survey for 24 Medi-Cal managed care plans. It is a figure with 5 plans on the vertical axis. The horizontal axis has percentages from 0-100 in 10% increments and is labeled with text saying "Percent of Appointments Available Within Timely Access Standards. There is a red dotted line at 90% that is labeled with text that says "Proposed Federal Standard." Each plan has two bars. One bar is blue, indicating the results for non-urgent appointments. The other bar is orange, indicating the results for urgent appointments. The first plan is labeled "San Francisco Health Plan (162,000 enrollees)." The non-urgent bar is at 99.6% and the urgent bar is at 98.8%. The next plan is labeled "Health Plan of San Mateo (133,000 enrollees)." The non-urgent bar is at 99.6% and the urgent bar is at 98.9%. The next plan is labeled "Santa Clara Family Health Plan (296,000 enrollees)." The non-urgent bar is at 99.4% and the urgent bar is at 54.4%. The next plan is labeled "Contra Costa Health Plan (230,000 enrollees)." The non-urgent bar is at 99.1% and the urgent bar is at 57.3%. The next plan is labeled "Partnership HealthPlan of California (654,000 enrollees)." The non-urgent bar is at 94.0% and the urgent bar is at 71.6%. The next plan is labeled "Kaiser (193,000 enrollees)." The non-urgent bar is at 93.5% and the urgent bar is at 75.3%. The next plan is labeled "CenCal Health (219,000 enrollees)." The non-urgent bar is at 88.1% and the urgent bar is at 72.3%. The next plan is labeled "Alameda Alliance for Health (308,000 enrollees)." The non-urgent bar is at 87.2% and the urgent bar is at 64.5%. The next plan is labeled "L.A. Care Health Plan (2,442,000 enrollees)." The non-urgent bar is at 81.4% and the urgent bar is at 46.3%. The next plan is labeled "Inland Empire Health Plan (1,515,000 enrollees)." The non-urgent bar is at 80.4% and the urgent bar is at 57.9%. The next plan is labeled "Gold Coast Health Plan (238,000 enrollees)." The non-urgent bar is at 80.3% and the urgent bar is at 86.7%. The next plan is labeled "CalViva Health (407,000 enrollees)." The non-urgent bar is at 76.9% and the urgent bar is at 58.4%. The next plan is labeled "Anthem Blue Cross Partnership Plan (926,000 enrollees)." The non-urgent bar is at 73.8% and the urgent bar is at 49.3%. The next plan is labeled "Molina Healthcare of California (515,000 enrollees)." The non-urgent bar is at 73.4% and the urgent bar is at 50.3% The next plan is labeled "Health Plan of San Joaquin (515,000 enrollees)." The non-urgent bar is at 68.2% and the urgent bar is at 44.5%. The next plan is labeled "Health Net Community Solutions, Inc. (1,561,000 enrollees)." The non-urgent bar is at 65.3% and the urgent bar is at 43.1%. The next plan is labeled "California Health and Wellness Plan (233,000 enrollees)." The non-urgent bar is at 63.2% and the urgent bar is at 39.3%. The next plan is labeled "CalOptima (898,000 enrollees)." The non-urgent bar is at 56.8% and the urgent bar is at 40.2%. The next plan is labeled "Blue Shield of California Promise Health Plan (121,000 enrollees)." The non-urgent bar is at 55.8% and the urgent bar is at 59.7%. The next plan is labeled "Community Health Group Partnership Plan (319,000 enrollees)." The non-urgent bar is at 51.6% and the urgent bar is at 43.2%. The next plan is labeled "Aetna Better Health of California (46,000 enrollees)." The non-urgent bar is at 47.9% and the urgent bar is at 45.9%. The next plan is labeled "Central California Alliance for Health (404,000 enrollees)." The non-urgent bar is at 44.5% and the urgent bar is at 49.2%. The next plan is labeled "Kern Family Health Care (333,000 enrollees)." The non-urgent bar is at 42.2% and the urgent bar is at 43.6%. The last plan is labeled "United Healthcare Community Plan (30,000 enrollees)." The non-urgent bar is at 25.1 and the urgent bar is at 0.0%. There is a note that reads "The percentage presented for each plan is the percentage of non-urgent and urgent appointments available within the timely access standards during DHCS' timely access survey. The percentages only include the survey results for therapists and are measured against a standard of 10 business days for non-urgent appointments and 96 hours for urgent appointments. As we discuss later, DHCS' use of the 96 hour urgent appointment standard for all therapist appointments is incorrect. Enrollment totals are as of June 2022."
Appendix B
Behavioral Health Services Delivered Per Beneficiary in 2022
Table B shows the variation in the average number of delivered behavioral health services per child beneficiary across the State for 2022. This detail was used to develop Figure 6 of the report.
Table B
Department of Health Care Services Claims Data for 2022
| County | Behavioral Health Services per Beneficiary |
| Alameda | 2.59 |
| Alpine | 3.21 |
| Amador | 2.31 |
| Butte | 2.72 |
| Calaveras | 3.37 |
| Colusa | 2.01 |
| Contra Costa | 3.15 |
| Del Norte | 2.60 |
| El Dorado | 3.45 |
| Fresno | 1.49 |
| Glenn | 1.90 |
| Humboldt | 3.13 |
| Imperial | 2.86 |
| Inyo | 1.26 |
| Kern | 1.31 |
| Kings | 1.35 |
| Lake | 2.36 |
| Lassen | 1.40 |
| Los Angeles | 2.47 |
| Madera | 1.05 |
| Marin | 2.10 |
| Mariposa | 2.13 |
| Mendocino | 3.49 |
| Merced | 1.35 |
| Modoc | 2.18 |
| Mono | 1.14 |
| Monterey | 1.64 |
| Napa | 2.70 |
| Nevada | 2.91 |
| Orange | 3.14 |
| Placer | 2.30 |
| Plumas | 1.86 |
| Riverside | 2.84 |
| Sacramento | 2.50 |
| San Benito | 1.04 |
| San Bernardino | 2.34 |
| San Diego | 2.37 |
| San Francisco | 2.58 |
| San Joaquin | 1.74 |
| San Luis Obispo | 3.27 |
| San Mateo | 2.06 |
| Santa Barbara | 1.90 |
| Santa Clara | 2.90 |
| Santa Cruz | 2.77 |
| Shasta | 2.49 |
| Sierra | 0.23 |
| Siskiyou | 2.15 |
| Solano | 2.25 |
| Sonoma | 2.19 |
| Stanislaus | 1.60 |
| Sutter | 1.83 |
| Tehama | 1.11 |
| Trinity | 2.11 |
| Tulare | 1.63 |
| Tuolumne | 2.17 |
| Ventura | 2.50 |
| Yolo | 2.49 |
| Yuba | 1.70 |
Source: DHCS claims data.
Appendix C
Children’s Emergency Department Visits for Behavioral Health Care, 2017 Through 2021
A 2022 report on behavioral health services in California prepared for DHCS cited survey and focus group results indicating that members sometimes seek behavioral health care from an emergency department when they cannot get an appointment with a Medi‑Cal behavioral health care provider in a timely manner.Manatt Health and Dr. Anton Nigusse Bland, Assessing the Continuum of Care for Behavioral Health Services in California: Data, Stakeholder Perspectives, and Implications, https://www.dhcs.ca.gov/Documents/Assessing‑the‑Continuum‑of‑Care‑for‑BH‑
Services‑in‑California.pdf, accessed August 29, 2023. The CDC has also reported that emergency departments are often the first point of care for children experiencing mental health emergencies, particularly when other services are inaccessible or unavailable.Leeb, Rebecca et al., Mental Health‑Related Emergency Department Visits Among Children Aged <18 Years During the COVID‑19 Pandemic—United States, January 1–October 17,2020, Weekly I, November 13, 2020, https://www.cdc.gov/mmwr/volumes/69/wr/mm6945a3.htm, accessed October 2, 2023. Using hospital emergency department and patient discharge data obtained from the California Department of Health Care Access and Information, we determined that during the five‑year period from 2017 through 2021, children in California visited emergency departments for behavioral health issues nearly 417,000 times—an average of more than 83,000 visits per year. Data show that Medi‑Cal was expected to pay for 52 percent of those visits, 37 percent were expected to be paid by private insurance, and the remainder were expected to be paid through another payment source such as Medicare. Table C includes the data on these visits by county. Overall, we did not identify a clear correlation between high instances of emergency department visits and lower numbers of behavioral health services provided to Medi‑Cal beneficiaries. However, these results do not mean that there is no relationship between serious untreated mental health conditions and emergency department visits. For example, we were unable to analyze the relationship between behavioral health wait times and emergency department visits because, as we discussed earlier in the report, there is no source of statewide data on appointment wait times. Nevertheless, the significant number of emergency department visits is generally consistent with the need for necessary improvements for timely access to behavioral health services for children enrolled in Medi‑Cal.
Table C
Emergency Department Visits for Behavioral Health Services by Children 20 Years Old or Younger
| County Name | 2017 | 2018 | 2019 | 2020 | 2021 | Changes from 2017 |
| Alameda | 3,377 | 3,438 | 3,444 | 2,663 | 2,818 | ▼ |
| Amador | 86 | 83 | 70 | 79 | 87 | ▲ |
| Butte | 764 | 663 | 611 | 414 | 480 | ▼ |
| Calaveras | 63 | 87 | 65 | 62 | 74 | ▲ |
| Colusa | 0 | 35 | 40 | 31 | 26 | ▲ |
| Contra Costa | 3,123 | 3,260 | 3,187 | 2,557 | 2,904 | ▼ |
| Del Norte | 116 | 114 | 117 | 98 | 108 | ▼ |
| El Dorado | 345 | 331 | 314 | 228 | 246 | ▼ |
| Fresno | 2,199 | 2,053 | 1,929 | 1,686 | 1,751 | ▼ |
| Glenn | 35 | 20 | 33 | 27 | 27 | ▼ |
| Humboldt | 345 | 277 | 302 | 309 | 273 | ▼ |
| Imperial | 354 | 299 | 352 | 242 | 257 | ▼ |
| Inyo | 43 | 40 | 48 | 48 | 50 | ▲ |
| Kern | 1,709 | 1,641 | 1,702 | 1,554 | 1,628 | ▼ |
| Kings | 640 | 584 | 664 | 466 | 517 | ▼ |
| Lake | 249 | 187 | 196 | 185 | 186 | ▼ |
| Lassen | 80 | 89 | 87 | 60 | 61 | ▼ |
| Los Angeles | 21,664 | 23,544 | 22,497 | 17,159 | 17,967 | ▼ |
| Madera | 881 | 834 | 916 | 770 | 814 | ▼ |
| Marin | 497 | 518 | 513 | 499 | 515 | ▲ |
| Mariposa | 44 | 47 | 35 | 15 | 33 | ▼ |
| Mendocino | 311 | 310 | 345 | 242 | 237 | ▼ |
| Merced | 561 | 500 | 507 | 447 | 486 | ▼ |
| Modoc | 16 | 16 | 21 | 12 | 17 | ▲ |
| Mono | 42 | 44 | 21 | 24 | 30 | ▼ |
| Monterey | 1,671 | 1,640 | 1,685 | 1,279 | 1,499 | ▼ |
| Napa | 168 | 159 | 181 | 159 | 158 | ▼ |
| Nevada | 212 | 197 | 210 | 208 | 228 | ▲ |
| Orange | 7,629 | 7,638 | 7,414 | 5,740 | 6,163 | ▼ |
| Placer | 1,519 | 1,568 | 1,456 | 1,320 | 1,346 | ▼ |
| Plumas | 43 | 49 | 56 | 42 | 43 | – |
| Riverside | 5,818 | 5,779 | 5,571 | 4,524 | 4,752 | ▼ |
| Sacramento | 2,895 | 3,071 | 3,313 | 2,660 | 2,745 | ▼ |
| San Benito | 180 | 167 | 171 | 112 | 146 | ▼ |
| San Bernardino | 4,828 | 5,189 | 5,381 | 5,441 | 5,015 | ▲ |
| San Diego | 8,038 | 6,785 | 6,767 | 4,954 | 5,671 | ▼ |
| San Francisco | 1,630 | 1,678 | 1,422 | 877 | 1,010 | ▼ |
| San Joaquin | 1,912 | 1,820 | 1,775 | 1,562 | 1,668 | ▼ |
| San Luis Obispo | 732 | 697 | 744 | 504 | 519 | ▼ |
| San Mateo | 1,264 | 1,233 | 1,251 | 909 | 953 | ▼ |
| Santa Barbara | 1,633 | 1,637 | 1,512 | 1,130 | 1,219 | ▼ |
| Santa Clara | 3,184 | 3,495 | 3,514 | 2,587 | 2,743 | ▼ |
| Santa Cruz | 614 | 546 | 559 | 435 | 459 | ▼ |
| Shasta | 471 | 441 | 484 | 366 | 382 | ▼ |
| Siskiyou | 116 | 131 | 106 | 104 | 81 | ▼ |
| Solano | 1,259 | 1,210 | 1,108 | 981 | 993 | ▼ |
| Sonoma | 1,195 | 1,211 | 1,225 | 992 | 1,031 | ▼ |
| Stanislaus | 1,274 | 1,424 | 1,163 | 1,066 | 1,098 | ▼ |
| Tehama | 119 | 107 | 102 | 88 | 103 | ▼ |
| Trinity | 27 | 20 | 27 | 19 | 25 | ▼ |
| Tulare | 1,148 | 1,014 | 1,274 | 1,218 | 1,125 | ▼ |
| Tuolumne | 141 | 154 | 171 | 127 | 136 | ▼ |
| Ventura | 1,691 | 1,679 | 1,724 | 1,384 | 1,675 | ▼ |
| Yolo | 580 | 579 | 551 | 446 | 440 | ▼ |
| Yuba | 313 | 345 | 369 | 296 | 347 | ▲ |
Source: Department of Health Care Access and Information’s emergency department and patient discharge data.
Note: There were no reported records of children visiting emergency departments for behavioral health primary diagnoses in Alpine, Sierra, and Sutter counties during our audit period.
Appendix D
Scope and Methodology
The Joint Legislative Audit Committee (Audit Committee) directed the California State Auditor to conduct an audit of the Department of Health Care Services (DHCS) and the Department of Managed Health Care (Managed Health Care) to determine if children enrolled in Medi‑Cal and California Children’s Services (CCS) receive timely access to behavioral health care. We were directed to determine, among other things, whether there was available statewide data related to children who sought behavioral health care and reasons for and effects of delays to children receiving behavioral health services. We were also directed to determine what steps DHCS and Managed Health Care could take to improve timely access for children. Table D lists the objectives that the Audit Committee approved and the methods we used to address them. Unless otherwise stated in the table or elsewhere in the report, all statements and conclusions about selections of items reviewed cannot be projected to the population.
Table D
Audit Objectives and the Methods Used to Address Them
| AUDIT OBJECTIVE | METHOD | |
|---|---|---|
| 1 | Review and evaluate the laws, rules, and regulations significant to the audit objectives. | Reviewed relevant federal and state laws, rules, and regulations applicable to access standards, including those for timely access, and DHCS’ and Managed Health Care’s oversight responsibilities. |
| 2 | Determine what statewide data is available related to children enrolled in Medi‑Cal or CCS who sought behavioral health care. If statewide data is unavailable, inspect health records for a selection of children enrolled in Medi‑Cal or CCS who sought behavioral health care services. |
|
| 3 | For children enrolled in Medi‑Cal or CCS, determine the following using statewide data for a selection of children:
|
|
| 4 | For a selection of children enrolled in Medi‑Cal or CCS who did not receive timely access to behavioral health services, to the extent possible, determine the reasons for delays in obtaining behavioral health services and the impacts of those delays on their care. |
|
| 5 | To the extent possible, determine how many behavioral health care providers in California accept Medi‑Cal. In Addition, determine how many behavioral health care providers provided services to Medi‑Cal patients in the last year. |
|
| 6 | Determine what steps DHCS and Managed Health Care can take to improve timely access to behavioral health care. | Obtained documentation and conducted interviews to evaluate DHCS’ and Managed Health Care’s methodology for timely access surveys. |
| 7 | To the extent possible, analyze emergency department visits for children needing behavioral health services for the most recent five year period to determine the following:
|
|
| 8 | Review and assess any other issues that are significant to the audit. | None identified. |
Source: Audit workpapers.
Assessment of Data Reliability
The U.S. Government Accountability Office, whose standards we are statutorily required to follow, requires us to assess the sufficiency and appropriateness of the computer processed information that we use to support our findings, conclusions, or recommendations. In performing this audit, we relied on data obtained from DHCS related to health care encounters and patient demographics. To evaluate these data, we performed electronic testing of the data, reviewed existing information about the data, and interviewed department officials knowledgeable about the data. We did not perform completeness or accuracy testing due to the fact that available source documentation would be located at individual medical providers throughout the State, making such testing cost prohibitive. As a result, we found the data to be of undetermined reliability. Although this determination may affect the precision of the numbers we present, there is sufficient evidence in total to support our findings, conclusions, and recommendations.
We also relied on data obtained from Department of Health Care Access and Information related to emergency department visits, patient discharges, and patient demographics. To evaluate these data, we performed electronic testing of the data, reviewed existing information about the data, and interviewed department officials knowledgeable about the data. We did not perform completeness or accuracy testing due to the fact that available source documentation would be located at individual hospitals throughout the State, making such testing cost prohibitive. As a result, we found the data to be of undetermined reliability. Although this determination may affect the precision of the numbers we present, there is sufficient evidence in total to support our findings, conclusions, and recommendations.
Responses
Department of Health Care Services
Department of Managed Health Care
Department of Health Care Services
November 3, 2023
THIS LETTER SENT VIA EMAIL.
Grant Parks
California State Auditor
621 Capitol Mall, Suite 1200
Sacramento, CA 95814
RE: RESPONSE TO DRAFT AUDIT REPORT 2023-115
Dear Mr. Parks:
The Department of Health Care Services (DHCS) hereby submits the enclosed response to the California State Auditor (CSA) draft audit report number 2023-115, titled, “Children Enrolled in Medi-Cal Face Challenges in Accessing Behavioral Health Care.”
In the above draft audit report, CSA issued nine recommendations for DHCS. DHCS has reviewed all of CSA’s recommendations and has prepared a response describing the nature of the corrective actions taken or planned.
DHCS is committed to improving and ensuring equitable access to all Medi-Cal members for Children’s Behavioral Health Services. On October 7, 2022, DHCS published the State Work Plan for Access Improvement documenting DHCS’ proposal to address the underlying factors impacting access. This Work Plan represents a robust, multi-faceted approach to assessing and improving access to care for Medi-Cal members across delivery systems. DHCS will perform an assessment of access overall, including a comparison of access to care measures across the commercial, Medicare, and Medi-Cal lines of business. In addition, DHCS enhanced access monitoring activities in 2023, including an assessment of Managed Care Plan subcontractors against federal and state network adequacy standards. California is leading the nation as the first state to undertake an assessment of this magnitude at the subcontractor level.
Specific to youth access to mental health services, as a part of California Advancing and Innovating Medi-Cal (CalAIM), DHCS implemented critical policy updates that expanded the population of Medi-Cal members under 21 years of age who meet access criteria for specialty behavioral health services (see Behavioral Health Information Notice 21-073 and All Plan Letter 22-006 describing Medi-Cal Managed Care coverage of non-specialty mental health services). DHCS, county behavioral health plans, and Medi-Cal Managed Care Plans have also implemented the “No Wrong Door” for mental health services policy (see Behavioral Health Information Notice 22-011 and All-Plan Letter 22-005). No Wrong Door enables Medi-Cal members to receive timely mental health services without delay regardless of the delivery system where they seek care and ensures that members are able to receive coordinated and non-duplicative mental health services from both delivery systems when needed and can maintain treatment relationships with trusted providers without interruption. DHCS will continue to monitor plan compliance and outcomes related to these policy changes, while also pursuing new opportunities to expand coverage and improve the quality of youth behavioral health services such as the California Behavioral Health Community-Based Organized Networks of Equitable Care and Treatment (BH-CONNECT) demonstration waiver that DHCS submitted for federal approval on October 20, 2023.
Additionally, DHCS is in the process of conducting a focused audit of all Medi-Cal managed care plans, regarding access to behavioral health services covered by Medi- Cal managed care plans. DHCS is assessing managed care plan processes and oversight mechanisms to determine if there are barriers to appropriate medically necessary covered services and the managed care plans’ provision of non-specialty mental health services, including coordination with the county mental health plan; processes for ensuring timely screening, assessment, and referrals; and oversight of its delegated subcontractor for providing non-specialty mental health services, if applicable.
DHCS appreciates the work performed by CSA and the opportunity to respond to the draft audit report. If you have any questions, please contact the DHCS Office of Compliance, Internal Audits at (916) 445-0759.
Sincerely,
Michelle Baass
Director & Interim State Medicaid Director
Enclosure
Cc: See Next Page
cc:
Lindy Harrington
Interim Chief Deputy Director
Health Care Programs
Department of Health Care Services
Lindy.Harington@dhcs.ca.gov
Erika Sperbeck
Chief Deputy Director
Policy and Program Support
Department of Health Care Services
Erika.Sperbeck@dhcs.ca.gov
Tyler Sadwith
Deputy Director
Behavioral Health
Department of Health Care Services
Tyler.Sadwith@dhcs.ca.gov
Susan Philip
Deputy Director
Health Care Delivery Services
Department of Health Care Services
Susan.Philip@dhcs.ca.gov
Saralyn Ang-Olson, JD, MPP
Chief Compliance Officer
Office of Compliance
Department of Health Care Services
Saralyn.Ang-Olson@dhcs.ca.gov
Wendy Griffe, MPA
Chief
Internal Audits
Department of Health Care Services
Wendy.Griffe@dhcs.ca.gov
Audit: “Children Enrolled in Medi-Cal Face Challenges in Accessing Behavioral Health Care”
Audit Entity: California State Auditor
Report Number: [2023-115] (23-17) (Behavioral Health Services for Children Audit)
Response Type: DHCS’ Response to CSA’s Draft Audit Report
Finding 1 Available Data Substantiate Long Wait Times to Access Behavioral Health Services for Many Children in Medi-Cal
Recommendation 1
To better ensure appropriate and effective monitoring of timely access to behavioral health care access for children, DHCS should do the following by November 2024:
- Determine the feasibility, costs, and likely benefits of adopting a “secret shopper” approach to their timely access surveys. If the departments determine that adopting such an approach is reasonably feasible and beneficial, they should implement this methodology by the next reporting year.
- Use their timely access surveys to monitor compliance with the two-day urgent appointment standard established in state law where applicable.
- Use their timely access surveys to monitor compliance with the timely appointment standards for both new and existing patients.
- Disclose the proportion of providers excluded from their survey results for each plan, the reasons for excluding those providers, and how such exclusions may affect the survey’s conclusions about access to care.
DHCS’ Response:
The Department of Health Care Services (DHCS) acknowledges the recommendation to conduct the feasibility analysis of a secret shopper approach by November 2024, and if determined to be feasible, implement the adjusted methodology by the next reporting year in 2026. As part of the feasibility analysis, DHCS will need to consider the operational steps needed when adjusting the methodology, which includes securing additional funding for the External Quality Review Organization (EQRO) to change the survey approach, working with the EQRO to test the new methodology, and providing guidance to implement the new process with Managed Care Plans (MCP) via an All Plan Letter (APL).
Every year, DHCS reviews and adjusts the survey methodology. DHCS currently surveys urgent appointments for some provider types and was already planning to expand the survey to include behavioral health providers in the two-day urgent appointment time category. The annual results of the Timely Access Survey will be published as part of the 2024 EQRO Technical Report, which will be published by April 30, 2025.
As part of the methodology adjustment, DHCS will explore implementing monitoring for both new and existing patients. This adjustment will be more involved as it will significantly impact the scope of the survey. This includes securing additional funding for the EQRO to change the survey approach, updating all call scripts and methodology, and working with the EQRO to test the updated methodology. DHCS will implement this change no later than the 2025 EQRO Technical Report, which is published by April 30, 2026.
DHCS will disclose the proportion of providers excluded from the survey, reasons for exclusion, and its impact to the survey by November 2024. The findings will be published as part of the 2024 EQRO Technical Report, which is published by April 30, 2025.
As described below, specialty behavioral health plans have historically reported timely access data in a standardized format rather than utilizing a survey method, and this reporting includes monitoring of urgent appointment standards for psychiatry. DHCS intends to adopt a survey method for behavioral health plans as part of the 2024 EQRO contract, and after undertaking the steps described above to explore and develop a new survey methodology, will align that methodology across managed care delivery systems to the extent possible.
Recommendation 2
To improve its ability to use timely access surveys as a tool to improve access to behavioral health services, by November 2024, DHCS should develop a compliance threshold for the percentage of appointments in each Medi-Cal plan meeting timely access standards. For example, DHCS might consider how many calls a member should have to make before obtaining a timely appointment and calculate a threshold accordingly.
DHCS’ Response:
DHCS agrees with this recommendation and has already been working toward developing and implementing compliance thresholds that are aligned across managed care delivery systems for 2024. DHCS is working internally to align across delivery systems and with the Department of Managed Health Care to establish consistent compliance thresholds. Once established, DHCS will set compliance thresholds and inform the MCPs of the policy by November 2024.
For specialty behavioral health services, DHCS already applies thresholds for compliance for all appointment types by age group, but will seek to align those thresholds with the standards for other managed care delivery systems as described above, and as needed will inform behavioral health plans of any resulting changes in compliance standards.
①DHCS requests that for this recommendation and throughout the report, where recommendations or findings refer to policies or methods that currently differ between managed care delivery systems, the California State Auditor (CSA) clarify the delivery system to which each finding, and recommendation is intended to refer.
Recommendation 3
To help determine whether timely access to mental health services for children is improving, by November 2024, DHCS should report in each year’s timely access survey results on the extent to which those results are comparable to previous years’ results and, where data is comparable, discuss the extent to which timely access to care is improving or declining.
DHCS’ Response:
For non-specialty mental health, DHCS will include the year-over-year trending methodology and work with the EQRO to update the reporting methodology by November 2024. DHCS had previously anticipated year-over-year trending in the EQRO report once the data was available. However, the COVID-19 Public Health Emergency (PHE) had systemic impacts to appointment availability, and subsequently, the ability to trend data from mid-2019 through 2022. DHCS will work with the EQRO to trend Timely Access Survey data starting with the 2023 and 2024 survey results. The findings will be published as part of the 2024 EQRO Technical Report, which is published by April 30, 2025.
For specialty behavioral health, the 2024 EQRO Technical Report (available in 2025 as described above) will be the first year in which a survey methodology is used to assess compliance with timely access standards. In past years, DHCS has instead required specialty behavioral health plans to report appointment time data in a standardized format, and has described this methodology in detail for CSA. Due to the planned change in methodology, DHCS will not be able to begin directly comparing year-over-year survey results until a second year of survey data is available from the 2025 EQRO cycle. However, DHCS generally agrees with the recommendation to analyze year-over-year changes in timely access results and to include that discussion in public-facing reports. DHCS will explore options to include this type of analysis in specialty behavioral health reports prior to having multiple years of survey data available (e.g., discussion of changes in overall rates of compliance may be incorporated even during the methodological transition).
Finding 2 Despite Compelling Evidence of Insufficient Provider Capacity for Children in Medi-Cal, DHCS’ Monitoring Efforts Demonstrate Weaknesses
Recommendation 4
To improve Medi-Cal members’ access to behavioral health services from county mental health plans and Drug Medi-Cal programs, by November 2024, DHCS should demonstrate that it followed up with county mental health plans and Drug Medi-Cal programs on CAPs that continue to be deficient in timely access of other network adequacy standards. In doing so, it should assess whether the plans took the action described in their CAPS’s and, if so, why those actions did not result in sufficient improvement.
DHCS’ Response:
②DHCS agrees with the recommendation and had already identified steps to improve the Corrective Action Plan (CAP) process prior to the CSA audit. For 2023 and subsequent submission cycles, DHCS will conduct ongoing follow-up with all plans that continue to be out of compliance after submitting a CAP for timely access and/or network adequacy standards. DHCS will require reporting from plans to ensure that plans are taking the actions that are specified in their CAPs to come into compliance with timely access standards. In addition to reporting on actions identified in CAPs, DHCS will require plans to resubmit data as needed to substantiate improvements to their networks. If plans fail to demonstrate sufficient progress or improvement via this process, DHCS will issue financial sanctions in instances DHCS deems appropriate.
Recommendation 5
To ensure that children in Medi-Cal have timely access to behavioral health services from county mental health plans and Drug Medi-Cal programs, by November 2024, DHCS should analyze county mental health plans and Drug Medi-Cal programs’ appointment data according to age group to determine if each county meets the compliance threshold for timely access for both adults and children. To the extent a plan does not meet timely access standards for either group, DHCS should require corrective action plan.
DHCS’ Response:
③DHCS agrees with this recommendation. Prior to the CSA audit, DHCS had recognized that there might be significant differences in timely access between the age groups and had already planned to begin analyzing the age groups separately. Beginning Fiscal Year 2024-25, DHCS will analyze county mental health plans’ and Drug Medi-Cal programs’ appointment data according to age group to determine if each county meets the compliance threshold for timely access for both adults and children. If plans fail to meet timely access standards for either group, DHCS will require CAPs from the plans to demonstrate how the plans will come into compliance with timely access standards.
Recommendation 6
To ensure that Medi-Cal managed care plans have a sufficient number of providers to offer timely access and meet children’s behavioral health care needs, by May 2024, DHCS should develop a new methodology for calculating non-specialty outpatient behavioral health provider-to-member ratios. At minimum, the methodology should consider the following factors:
- The expected demand for behavioral health services by children in Medi-Cal, based on factors including but not limited to past services.
- The estimated number of children likely to need those services.
- The number of full-time providers needed to provide that volume of services.
- The amount of time individual providers spend seeing Medi-Cal members.
The methodology should also accommodate potential growth in the need for behavioral health services.
DHCS’ Response:
DHCS has already initiated a work effort to update the non-specialty outpatient behavioral health provider-to-member ratios methodology as part of improvements to the annual network certification (ANC) process. This update will be included in the 2024 ANC. By May 2024, DHCS will conduct an analysis to consider the above recommended factors and update the provider-to-member ratio methodology accordingly. In developing the methodology, DHCS will consider the feasibility of each of the recommended factors based on available data. If feasible, the methodology will include the recommended considerations, which include expected demand, estimated utilization, and projected number of providers in a statistically significant way.
Recommendation 7
To ensure that Medi-Cal members do not have to travel unreasonable times or distances to receive care, DHCS should develop a definition of what times and distance are reasonable for Medi-Cal Members to travel. In doing so, DHCS should consider both the total time or distance a member needs to travel, as well as how those times and distances compare to other plans’ times and distances for the same provider type and Zip code. Having done so, when DHCS determines that plan’s requests for alternative time and distance standards are not reasonable, it should not approve those alternative access standards, thereby requiring those plans to offer members out-of-network access until such time as the plans can provide reasonable times and distances.
DHCS’ Response:
In 2022, DHCS published the State Work-Plan for Access Improvement documenting DHCS’ proposed process for assessing access, addressing the underlying factors impacting access, and the steps DHCS will take to improve access. DHCS began development of the access improvement results reporting and is working towards assessing access across multiple lines of business (i.e.,Medicare and commercial). DHCS is performing comprehensive analyses aimed at evaluating access to care and addressing concerns overall, including Alternative Access Standards (AAS). The outcomes of these efforts will result in updated processes and procedures. As part of those updated processes and procedures, DHCS will develop and document reasonableness standards to be used during the AAS approval process. If MCPs do not meet the reasonableness standards, AAS will be denied. DHCS will require MCPs without an approved AAS to provide out-of-network (OON) access to impacted members. MCPs without approved AAS will be subject to technical assistance, corrective actions, and/or further enforcement action. DHCS already initiated actions to advance this recommendation by instituting the subcontractor network certification (SNC) compliance process with the goal of improving network adequacy and access to care for Medi-Cal members. The SNC requires MCPs to assess subcontractors for compliance with network adequacy and access standards, hold those subcontractors accountable via corrective action plans and enforcement, and report results to DHCS. DHCS understands that California is the first state in the nation to hold MCPs responsible for enforcing network adequacy and access standards with subcontractors. To the extent possible, this policy will be aligned across managed care delivery systems and can be adopted for specialty behavioral health as well.
Recommendation 8
To ensure that plans make efforts to obtain additional providers to meet network adequacy standards, by May 2024, DHCS should revise its agreements with plans that do not meet time and distance standards to require them to demonstrate efforts to recruit new providers to underserved areas.
DHCS’ Response:
DHCS acknowledges increasing the number of physicians that practice in California would be beneficial for all health care delivery systems. DHCS contractually requires MCPs to ensure and monitor an appropriate provider network within its service areas in compliance with network adequacy standards, and if necessary, attempt to contract with providers in adjoining counties outside of their service area. To strengthen this further, no sooner than contract year 2025, DHCS will contractually require that MCPs that do not meet compliance with specified network adequacy requirements to demonstrate efforts in recruiting new providers to underserved areas. The same contract requirements and considerations apply for specialty behavioral health plans.
Recommendation 9
To more effectively encourage plans to comply with network adequacy standards by May 2024, DHCS should develop and implement a policy outlining when a plan’s noncompliance with network adequacy standards justifies financial penalties.
DHCS’ Response:
DHCS has broad enforcement authority established in state and federal statute to ensure compliance with network adequacy and access standards. DHCS has already issued APL 23-012 to further clarify compliance mechanisms, including monetary sanctions. DHCS convenes a Department-wide Enforcement Committee as a forum to raise MCP performance concerns cross-divisionally and build a consensus on the appropriate enforcement actions across program areas. By May 2024, DHCS will develop and implement a policy outlining when financial penalties are the appropriate enforcement mechanism for non-compliance.
⑤As previously communicated to CSA, for specialty behavioral health delivery systems, DHCS published Behavioral Health Information Notice (BHIN) 22-045 in August 2022, which describes DHCS’ authority to impose administrative and financial sanctions on behavioral health plans for an array of contractual infractions, including but not limited to noncompliance with network adequacy standards. DHCS has subsequently developed internal policies to establish standardized procedures for applying financial penalties specifically for noncompliance with network adequacy standards, and will implement these procedures as part of the 2023 annual network adequacy certifications for specialty behavioral health plans.
California State Auditor’s Comments on the Response From The Department of Health Care Services
To provide clarity and perspective, we are commenting on DHCS’ response to our audit. The numbers below correspond to the numbers we have placed in the margin of its response.
①As is our standard practice, we communicated with DHCS while it was reviewing the draft report to discuss any concerns it may have. During these conversations, DHCS requested clarification regarding the delivery system to which we directed specific findings and recommendations, and we informed DHCS that we would make minor edits to relevant findings and recommendations in our final report to provide that clarification.
②During the course of our audit we learned that DHCS had identified steps to improve its Corrective Action Plan process prior to the commencement of our audit. However, because it had not yet implemented those steps, we worked with DHCS to inform our recommendation that it develop and implement a policy outlining when noncompliance with network adequacy standards by a Medi-Cal managed care plan, county mental health plan, or county Drug Medi-Cal program justifies financial penalties.
③We agree that before the commencement of our audit, DHCS recognized its survey data shows that the availability of timely access can differ between age groups, which we acknowledge. However, during the course of our audit, we learned that DHCS had not yet analyzed county mental health plans’ and Drug Medi-Cal programs’ appointment data according to age group. It also did not require corrective action when a mental health plan did not meet timely access standards. Thus, we recommend that DHCS perform such an analysis and hold plans accountable that do not meet timely access standards.
④DHCS’ response does not address our recommendation that it determine the number of mental health providers a managed care plan has available to serve children in Medi-Cal by considering whether providers serve multiple plans or multiple regions within a single plan, and then accounting for that overlap. We look forward to reviewing DHCS’ response to that recommendation as part of its 60-day response.
⑤In its response, DHCS describes notices it issued to plans to communicate its authority to impose financial sanctions. Although this communication is a step in the right direction, our recommendation is that it develop and implement a policy outlining when noncompliance with network adequacy standards by a managed care plan, county mental health plan, or county Drug Medi-Cal program justifies financial penalties.
Department of Managed Health Care
November 3, 2023
VIA ELECTRONIC MAIL
Grant Parks
California State Auditor
621 Capitol Mall, Suite 1200
Sacramento, CA 95814
Re: DMHC Response to CSA Report 2023-115: Children Enrolled in Medi-Cal Face Challenges in Accessing Behavioral Health Care
Dear Mr. Parks:
The Department of Managed Health Care (DMHC) is committed to ensuring that health plans provide each enrollee timely access to the full range of health care services, including children seeking critical behavioral health services. The mission of the DMHC is to protect consumers’ health care rights and ensure a stable health care delivery system.
The DMHC appreciates the CSA’s recommendations for ways to improve the methods health plans use to monitor and report on their compliance with timely access requirements via the annual Timely Access Compliance Report. In particular, the DMHC is interested in exploring the feasibility of using data tracked in provider practice management software to collect actual appointment wait time information.
①However, the CSA’s recommendations primarily relate to potential changes to the timely access survey methodology that health plans are mandated to use to monitor compliance with timely access standards. This methodology was enacted into a regulation by the DMHC via formal rulemaking in April 2022 after five years of testing variations of the methodology with health plans under an exemption from the Administrative Procedure Act (APA) granted by the legislature in Senate Bill (SB) 964 (2013-2014 Sess.). The legislature recognized in SB 964, and again more recently in SB 221 (2021-2022 Sess.), that the DMHC cannot make changes to the methodology without first testing and refining the approach to ensure the feasibility of the change and to confirm the change results in reliable, valid, and comparable data. To fully implement and refine CSA’s recommended changes to the methodology, and provide health plans with appropriate notice of the changes so they can be implemented and tested during the Measurement Year, the DMHC would require the legislature to enact an extensionof the exemption from the APA set forth in Health and Safety Code section 1367.03, sub. (f)(3).Health and Safety Code section 1367.03, sub. (f)(3). provides the DMHC with the authority to make changes to the methodology without going through the formal rulemaking process until December 31, 2025.
②To be clear, the DMHC uses a variety of regulatory oversight tools to achieve its mission and ensure enrollees receive timely access to care. The CSA report specifically addresses the DMHC’s timely access oversight efforts associated with the receipt and review of health plans’ Timely Access Compliance Reports. That process includes reviewing all monitoring information submitted in health plans’ Timely Access Compliance Reports and annual publication of the timely access report to the DMHC’s public website. DMHC also oversees timely access to care in other ways, including: resolving and monitoring enrollee complaints submitted to the DMHC Help Center to identify trends, performing network adequacy reviews annually and on an ad hoc basis, auditing of health plan operations through routine medical surveys, conducting behavioral health investigations of commercial full service health plans, and taking enforcement action against health plans that violate timely access requirements, which may include administrative penalties and corrective action.
Sincerely,
Mary Watanabe
Director
Department of Managed Health Care
California State Auditor’s Comments on the Response From The Department of Managed Health Care
To provide clarity and perspective, we are commenting on Managed Health Care’s response to our audit. The numbers below correspond to the numbers we have placed in the margin of its response.
①Managed Health Care’s response implies that to implement our recommendations related to making changes to its survey methodologies would require a legislative extension of its existing exemption from the Administrative Procedure Act (APA). However, it is unclear how this relates to our recommendation that Managed Health Care simply make changes to its survey methodology by November 2024 and then implement those changes for the subsequent reporting period. Managed Health Care’s current exemption from the APA does not expire until December 2025. To the extent that Managed Health Care is unable to ensure the feasibility of the changes and to confirm the changes result in reliable, valid, and comparable data over the next two years, then it may choose to request that the Legislature extend the exemption.
②We acknowledge that Managed Health Care oversees timely access to care in other ways, including by reviewing complaints and medical surveys, and performing network adequacy reviews. However, we do not believe that these activities are a substitute for using its surveys to monitor compliance with timely access standards.